Misuse of Misoclear driving abortion rates
“One morning, in December last year, as the taxi I was travelling in came to a halt on Nakivubo Road, my eyes landed on a poster on the wall of BAPS Shree Swaminarayan Mandir Temple (Biwologoma). Someone was advertising legal abortion services. This seems interesting, I thought to myself.
When I called the telephone number provided on the poster, a man answered. He was cordial, and when I told him I wanted to have an abortion, he asked, Is this your first time to call this number? When I answered in the affirmative, he promised to send me a price list so that I would go to the clinic near Nakasero Market with an informed view.
Five minutes later, he sent an SMS. An injection, which begins to work within 35 minutes of being administered, costs Shs194,500. A pill, which takes 45 minutes to induce the abortion, costs 167,000. The vacuum clean, which removes the fetus in 17 minutes, costs Shs236,000. Cleaning the womb after the abortion is free of charge.
In Uganda, abortion is illegal, except when the pregnancy is endangering the woman’s life or her mental health. However, the demand for induced abortions seems to be on the rise. In rural areas, this could be attributed to the 40 per cent unmet need for family planning services.
In urban areas, though, where there is an abundance of family planning services, the rise in abortions is an enigma.
Ease of obtaining an abortion
A similar abortion advert – with cheaper prices – almost cost Sarah Nabuso her life. In July 2016, the 28-year-old salesgirl, was kidnapped by her boyfriend. The relationship was a violent one and she had been trying to get out of it, in vain.
He drove her to a house in Mutungo and for four months, kept her in solitary confinement. In October, she managed to escape from him. She was four months pregnant.
“I hated that pregnancy,” Nabuso says, continuing, “I did not want his baby. When I confided in a friend, she told me about a clinic downtown where I could get abortion tablets. She said it would not hurt; it would be like having my (menstrual) period.”
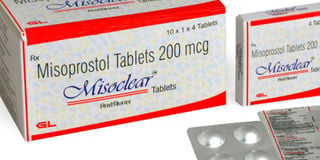
Her friend had used the services of the said clinic twice. When Nabuso visited the clinic, the doctor gave her a small box containing four tablets. “The box was labelled Misoclear and cost Shs15,000. He told me to put two tablets under my tongue and push the other two deep inside my vagina.”
The misuse of Misoclear
Misoclear, a brand produced by Marie Stopes International, is recommended by World Health Organisation (WHO) as a highly effective drug for preventing heavy bleeding after childbirth. In Uganda, Misoclear is sold under the names Misoprostol and Cytotec.
Misoprostol was imported into Uganda for research use in 2002. On June 25, 2008, the National Drug Authority (NDA) licensed the use of the drug for prevention of post-partum hemorrhage. In 2012, NDA included misoprostol on the Essential Medicines List.
Annet Kyarimpa, the technical coordinator for safe motherhood at Reproductive Health Uganda (RHU), says any drug that is bought without prescription is dangerous.
“Misoprostol is a life-saving drug that is used to manage miscarriages or incomplete abortions if the products of conception (fetus) are not completely expelled (from the uterus),” Kyarimpa says, adding, “It can also be used to induce labour in women who have gone beyond their term. It also induces abortions, and this is where it is being misused.”
The box in Nabuso’s hands clearly indicated that the tablets should only be used on a two-month pregnancy but the doctor assured her that they could also work on a four-month pregnancy. She used the drugs as instructed and then, boarded a taxi to Mukono to visit a friend, Maryann Nabankema.
“Misoprostol is being misused because the regulators (NDA) do not restrict over-the-counter procurement of drugs,” Kyarimpa says, continuing, “This is a drug that should be taken under observation (of a health worker). Different doses of the drug are prescribed according to the stage of pregnancy. But, girls are advising their friends to use Misoprostol and no one is talking about the dosage.”
To show how fatal misoprostol can be, Kyarimpa talks about a midwife in Mbale District whose pregnancy was overdue. She self-prescribed the drug to induce labour, took an overdose, and died from a raptured uterus.
Disaster strikes
Nabuso spent the night at her friend’s home because she was nervous about the abortion. At about 1.30am, Nabankema, woke up and turned on her side in the bed they were sharing.
“My hand touched some wetness,” she says, continuing, “I switched on the light and saw blood. Sarah’s eyes were wide open but she could not move or speak. So much blood was flowing out of her.
I thought she was having her periods. I did not have (sanitary) pads, so I went to the 24-hour clinic in front of my landlord’s house and asked the nurse to lend me a cotton roll.”
Nabankema explained Nabuso’s condition to the nurse. “She wondered what kind of periods those were. We walked back to the room and found Sarah on the floor. I think she had tried to follow me to explain what was happening. There was so much blood on the floor. Her eyes were sunken and her hands were turning yellow.”
The nurse ran to a neighbour’s home and woke them up, begging them to drive the young woman to Namirembe Hospital. She pushed a huge wad of cotton between Nabuso’s legs and the two women carried her outside. By the time they reached the car, the cotton was dripping with blood.
Although it is a life-saving drug, misoprostol can also be fatal. Kyarimpa says, “Many girls are dying but the cause of death is not documented. A girl will die in her bed, in a pool of blood, but no one will know what happened. Some girls take repeat doses; if the tablets do not work, they take more, and this is dangerous because if the pregnancy continues to term, the foetus does not develop normally.”
Saving Nabuso’s life
At Namirembe Hospital, the nurse on duty asked for Shs60,000, the fee charged for deliveries. Nabuso would be treated as a delivery case. “She stuffed some tablets into her mouth, probably to stop the bleeding,” Nabankema says, adding, “Then, the doctor came took her to the labour ward and put her on a drip to induce labour.”
During the abortion, one half of the fetus had come out. After one hour on the drip, Nabuso went into labour and pushed out the other half of the baby. She was placed on a two-month dose of antibiotics.
Intriguingly, two months after her ordeal, Nabuso made up with her abusive boyfriend and got pregnant. She now has a five-month-old baby girl.
However, even though misoprostol is sold freely on the market, many health centres (II and III) do not have it. It is only stocked in major hospitals where midwives have been trained to use it.
Kyarimpa advises, “Misoprostol is a good drug because it has saved the lives of many women with postpartum bleeding. However, NDA should regulate its procurement. No one should be able to buy the drug without a prescription.”
Nabuso is one among the large number of girls and women – including sex workers – misusing misoprostol. These women need to be advised to seek contraceptive methods that suit them rather than self-prescribing misoprostol five times a year.
Statement from National Drug Authority
“Misoprostol is registered in Uganda by NDA as a prescription-only medicine (POM) so it can only be sold or dispensed with a valid prescription from a medical doctor.
Pharmacies have professional staff under the lead of a pharmacist who are aware that misoprostol is a POM and should only be dispensed when a patient presents a valid prescription. Those who sell it without a prescription risk losing their license, as such a practice is against the law. NDA conducts sensitisation activities to sensitise the public about the danger of inappropriate use of different medicine.
We urge the public to be vigilant against unscrupulous operators in the pharmaceutical sector and report such incidents on our online platforms, including the toll free 0800101999.”
Frederick Sekyana
Head of Public Relations, National Drug Authority.
Abortion rates in Uganda
According to a study conducted by the Guttmacher Institute and Makerere University Incidences of Induced Abortion in Uganda, 2013: New estimates since 2003, whose results were released in February 2017, an estimated 314,300 women had induced abortions in 2013.
The study also found that 93,300 women were treated across the country for complications from unsafe abortions.
“Those numbers represent only women who come to health facilities when the abortion goes wrong,” says Annet Kyarimpa, the technical coordinator for safe motherhood at Reproductive Health Uganda.
Many abortions undocumented
Kyarimpa adds, “There are many successful abortions that are not documented. However, it is true that abortion is the leading cause of maternal mortality, with some dying as a result of over bleeding or post-abortion infections.”
The study also found that 52 per cent of all pregnancies in Uganda in 2013 were unintended and about a quarter of these unintended pregnancies ended in abortion.




