Handling the delicate period after a c-section

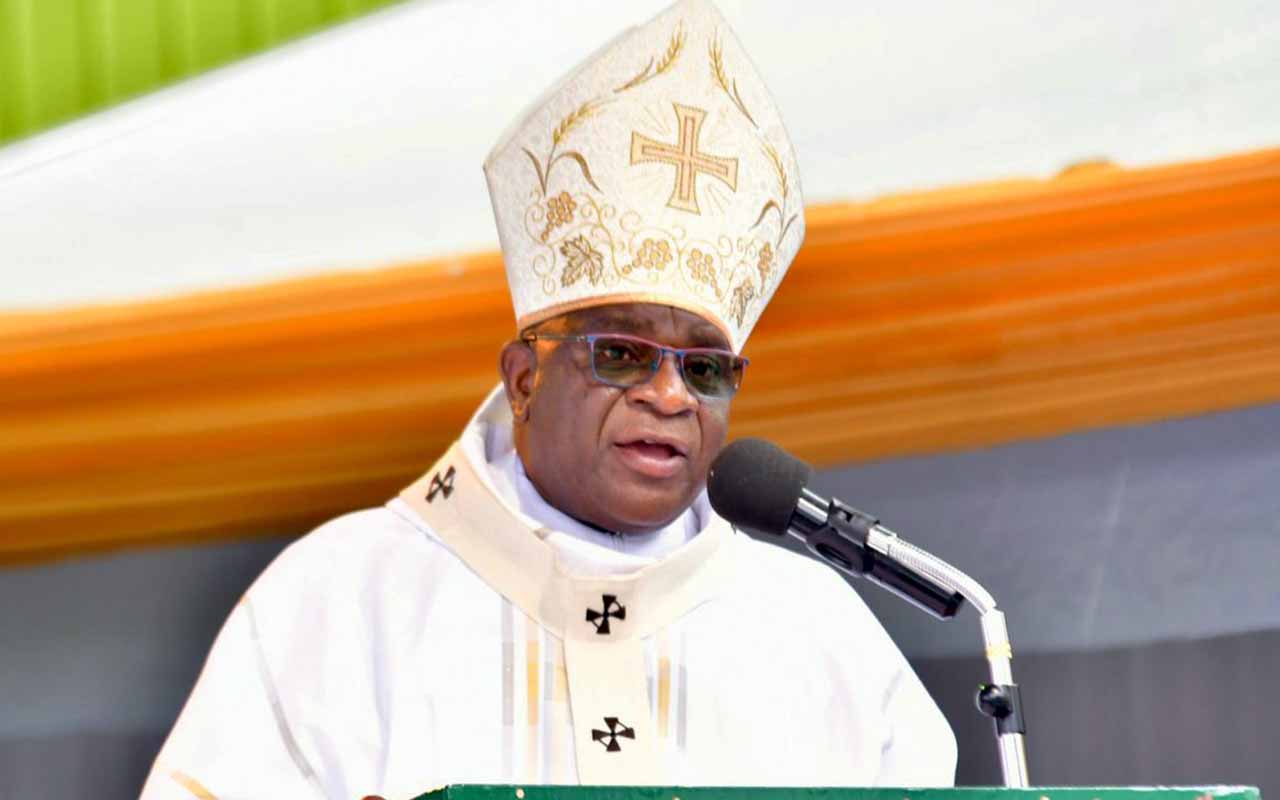
For a mother who has had a caesarian section, it is advisable to wait for at least six weeks before attempting to drive a car. photo by Rachel Mabala.
What you need to know:
The first few days after a caesarian section are the most dangerous for a new mother. Ironically, this is the time when many mothers and caregivers let down their guard as they celebrate the arrival of the newborn child.
Many new mothers, and their caregivers consider that the danger is over after the baby has been safely delivered and they are eager to go back home after a short stay in the hospital. That was how it was for Sharifa Nagayi.
After a prolonged labour of three days in a clinic, Nagayi was referred to a hospital and operated on immediately.
Two days after her caesarian section, she managed to convince her doctor to discharge her. She could walk around without support and could even carry her baby.
“Two days after being discharged I realised the bandages around the incision were wet with a light liquid. I was having severe headaches and was sweating profusely.” Nagayi recalls.
Nagayi was in great pain when her boyfriend convinced her to see the doctor, who discovered that the surgical incision had been infected.
Postpartum mortality
Dr Robert Busingye, a senior consultant obstetrician and gynaecologist at Mulago hospital, says that the first few days after delivery are the most dangerous for a new mother.
“The body system normally goes back to normal six weeks after delivery but that six week period, especially the first week, is the most dangerous; especially for those who had complications before delivery.”
Anaemia
Complications such as postpartum haemorrhage (bleeding) can manifest or get worse days after delivery. The new mother may have been anaemic before delivery and may bleed excessively after giving birth.
“Measuring the amount of blood lost is difficult because the patient may continue to bleed from a point of weakness. She (a mother) may bleed after the operation, then continue to bleed a little in the next few days, and then heavily again. It is the little amounts of bleeding that tilt the scale,” says Busingye.
There is more blood lost during a caesarean birth than in a vaginal birth, and sometimes assessments concerning the blood lost may be underestimated.
Severe anaemia can lead to heart failure, infections since the immune system is low and death if not attended to immediately.
Infections
With C-sections, the risk of contracting infections is quite high because the incision goes through the abdominal wall and cavity, to the uterus.
The risk is higher in women who have gone through a prolonged labour before the decision to operate is made. By this time they have gone through many physical examinations to check dilation and in this way bacteria may be introduced. Sometimes, their membranes have already raptured.
In medical terms, labour that goes beyond twelve hours is considered to be prolonged. For emergency C-sections, infections may manifest after the woman has left the hospital.
Some infections are external and appear only on the surface of the incision. Busingye says that these are not life threatening as compared to internal infections, where “the bacteria spread to the uterus and other internal organs. If the infection gets into the blood stream, it can lead to death,” adds Busingye.
In a planned C-section, the risk of infection is low because the dates and time for the operation are agreed upon and known by both the patient and doctor.
Pre-eclampsia
Although not unique to women who have gone through caesarean births, a late onset of hypertension may occur. Hypertension before delivery may go down after the operation, but sometimes it does not.
Postpartum eclampsia can lead to pneumonia and even death.
Pain management
As in any other medical procedure, pain after the operation is better prevented than treated. Pain management needs to start in the operating theatre.
“The medical team needs to balance different medicines that are to be administered before the pain sets in,” says Dr Busingye.
Pain medication can be administered through injections or by rectal tablets. Upon being discharged from hospital, painkillers should be orally administered.
With pain management, the first three days after the operation are crucial. If well managed, then the requirement for more drugs after discharge is low.
Individual variations should be taken into consideration.
What to look out for
For mothers who have had a caesarian section, a hospital should give a discharge note which indicates the alerts that a mother should pay attention to.
Severe dizziness and weakness, and a rapid heartbeat are signs of anaemia.
For infections: the mother should look out for;
severe headaches,
fevers with a temperature higher than 37 degrees Celcius and
profuse sweating.
A foul-smelling vaginal discharge and abdominal swelling, with the incision turning red, are also signs of infection.
With hypertension, the signs are severe headaches, difficulties with sight, and convulsions.
Any of these signs are an emergency that should be attended to.
When to be active
The patient should gradually become active to prevent blood clots from developing in the veins.
“Walk about in the hospital after the surgery and continue to do so even after going home,” says Dr Busingye, adding, “It does not cause any harm and as long as you do not lift heavy objects, other activities are okay if there is no pain involved.”
For driving, however, the gynaecologist advises the mother to wait at least six weeks after the operation.
care for the surgical incision
“Infection usually comes from within, and as with these kinds of infections, the patient really has no control over them. Infections are introduced if the surgical infection prevention processes are not followed, ” says Dr Robert Busingye, a consultant obstetrician.
Surgery should be done in a sanitised place with sterilised equipment. Proper pre-skin preparations must also be done on the patient, who must have a good bath before the surgery.
“The patient only has the ability to prevent the minor infections that may set in after they are at home. They should keep the dressing around the wound dry until the doctor removes it.”
Immediately after the c-section, one should only have dry baths or cloth baths with a minimum of water used. With good progress, one can have a normal bath after seven to eight days when the bandages are removed, although one should not scrub the scar while bathing.
Busingye recommends constant evaluations of the incision for signs of infection. This must be done by the doctor.
“Prophylactic antibiotics may be given to prevent infection, after evaluation by the doctor, but when there is a low risk of infection, there is no need to use antibiotics three days after the surgical procedure,” he adds.
Real life experiences
“My C-section was planned two weeks before it was performed. During a routine checkup at SAS Clinic, the doctors discovered the umbilical cord was coiled around the neck of the foetus. This being my first child, they were honest with me and told me that a normal vaginal birth was risky.
I was scared but they encouraged me that the operation would be fine. Some of the doctors had also given birth through C-section so I was encouraged. The operation was performed using regional anaesthesia so I was awake while it was happening. The healing process was long and gradual.
The first two days after the operation, I had a severe headache and could not move. The breast milk did not come for a long time. For the first three months, I had difficulty walking. I felt a lot of pain but I was given painkillers and advised against doing strenuous work, sitting and bending for long periods of time. Luckily I had people around me who helped me do most of the work in those months.
My first review with the doctors was a week after the surgery and when the prognosis was good, they removed the bandages. I had my first bath in a week.”
Judith Mabeli
Housewife, Entebbe, Wakiso District
“I was in my last month of pregnancy when all of a sudden, the labour pains hit me. There were no warning signs. Two months earlier, I had gone to the health centre but since I was feeling okay, the nurse told me to come back another day. This was my seventh pregnancy.
When the pain started, I walked to the health centre and after examining me, the nurse said the labour was progressing well.
Two days later, I had not given birth and I was in terrible pain. The nurse later told my husband that one of us would die – either I or the baby. She advised him to take me to Entebbe Hospital immediately. It was midnight and there were no taxis on the island where we live.
Luckily, my husband has a motorcycle so he rode me to the landing site. But there were no boats travelling across the lake at that time. The only fisherman willing to take us asked for shs 50,000. When we reached the hospital, I was taken into theatre after three hours and a C-section performed.
Both the child and I are fine. However, since I had prolonged labour, I feel a lot of pain and general body weakness. I was given painkillers but the pain is intense.
By the second day after the operation, I could walk but with a lot of difficulty. I had to use the bed and the walls for support. However, I was told that this is normal and the healing process is gradual.
I am only scared of the ride on the boda boda from the lake to my home because the road is bumpy.”
Sharifa Tilusonyiwa
Trader, Bussi Island, Wakiso District
Diet after c-section
Since the intestines are not operated on during a C-section delivery, some women can quickly return to their normal diets,” says Busingye. “However, for some, the intestines do not work well, so gas may build up in the stomach, causing discomfort. For gas, according to the doctor’s prescription, a patient may take antacids, magnesium tablets or charcoal tablets.
A few days after the operation, the patient may develop constipation. For such cases, it is advisable to eat a lot of fluids, vegetables and fruits to ease the system.