Why treatment of mental illness in northern Uganda is failing

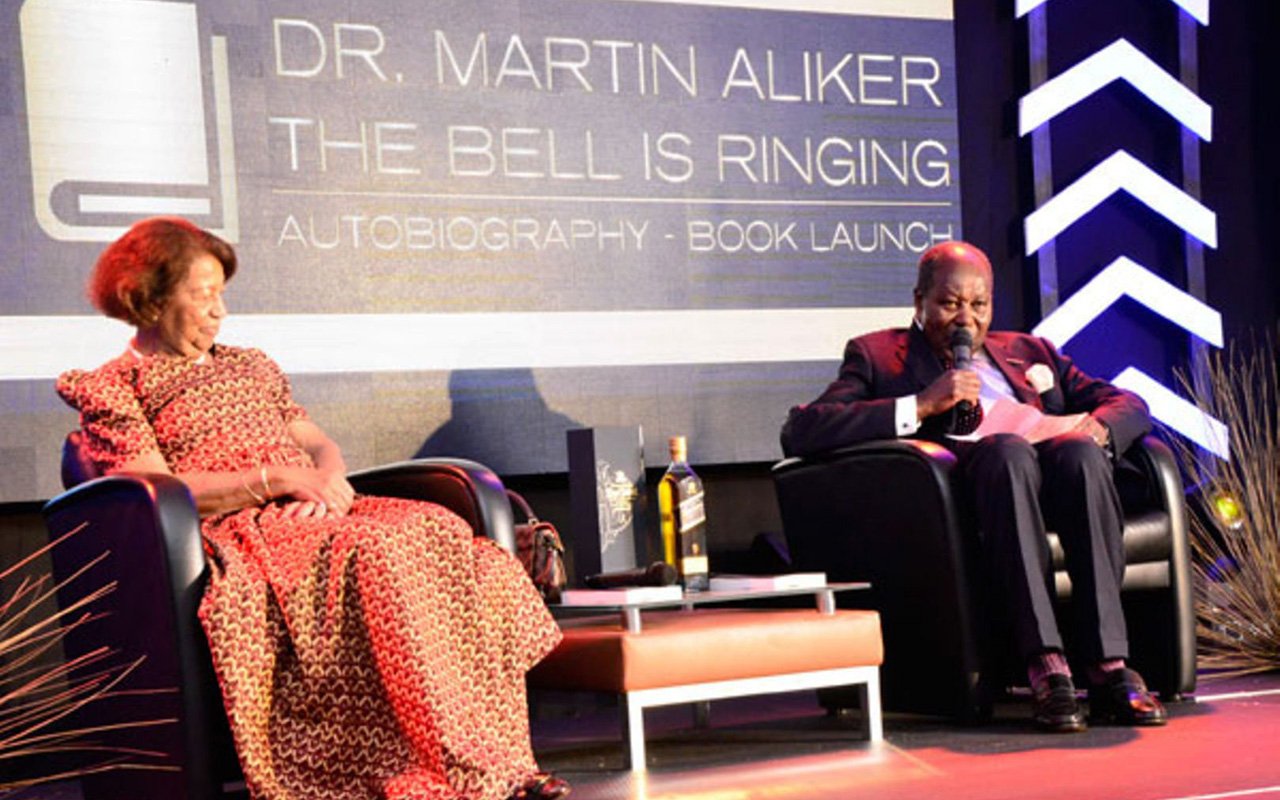
David Martin Aliker (left) chats with Robert Kidega at his home in Gulu. Photo by Caroline Ayugi
When Robert Kidega of Panyikwara village, Bungatira Sub-county in Gulu District broke down with bipolar disorder (a brain disorder that causes unusual shifts in mood, energy, activity levels, and the ability to carry out day-to-day tasks) in the year 2000, his family abandoned him to eating in garbage skips and sleeping in a dilapidated structure.
Before the onset of the disease, Kidega had succeeded in his education and eyed a bright future. After sitting for his primary leaving examinations in 1992 from Negri Primary School, he joined St. Mary’s College Kisubi and was later admitted on government scholarship to study bachelor of Laws at Makerere University. However, after only one semester, he dropped out and went back to his village, where he lived without medical care or support from his family and the community.
When David Martin Aliker, his former classmate, met him in 2012, Kidega was unrecognisable with tattered clothes and unkempt hair.
“There were all signs that he had been ill for a while and without any care. Residents showed me the rubbish pits that had become his one place to get something to eat and a dilapidated house in which he slept,” Aliker says.
His family members had a firm conviction that his mental problem was related to witchcraft, and could not be managed by conventional medicine.
Help
Aliker took the fight to Facebook where he published his friend’s plight with the hope of garnering assistance from their former classmates and other well-wishers. However, although Shs3 million was collected, it took a lot of persuading for the family to allow Aliker to take Kidega to Butabika Hospital, saying it would be a waste of time and money.
The friends won the day and took Kidega to Butabika Hospital where after receiving treatment for six months, he returned to his normal ways and was allowed to go back to his village. However, the continued lack of nutritional and psychosocial support from his family led to a relapse. Although he was accommodated at his in-law’s house, Kidega has since relocated to an abandoned house, where he stays alone, citing mistreatment from his in-law.
Kidega’s paternal uncle, Stanislao Okony, 89, says he cannot help Kidega since he himself is dependent on his daughter. Okony is quick to say that he [Kidega] can be persuaded to resume staying with his in-law, “if Aliker offers financial support for to buy him food.”
Lilly Grace Lanyero, a clinician at the Mental Health Unit of Gulu Referral Hospital, says Okony’s statement is typical of many families in the region who have members suffering from mental illness. According to Lanyero, the statement reflects how families are unwilling to part with money to provide medication, and even the most basic necessities to patients of mental illness.
“Many patients say they miss their review dates because they lack transport or are kept busy by family members doing several chores.”
Culture
Lanyero attributes the low management of mental health problems in the region to different cultural beliefs saying: “People still attribute mental health to witchcraft, curses and spirits of the dead. These beliefs, she says, make mental health patients not adhere and affects their healing process.”
According to Lanyero there is little psycho-social support from family members and the community. “On a weekly basis, we register complaints by patients of being overworked and insulted by members of their family. This leads to withdrawal and therefore relapses,” she adds.
Study
A 2014 study by John Paul II Justice and Peace Centre titled ‘Drugs, spirits and human rights: Mental Health in post-conflict Northern Uganda in the context of modernisation and traditional beliefs”, states that cases reported where families lock or chain their relatives with mental illness seem to be more common than those where people suffering from mental illness are abandoned to roam the streets.
According to the study, the sick relative is perceived as a burden, families give up on them, while those who are physically fit are exploited and forced to work leading to breakdown or exhaustion.
Dora Single Alal, is a counsellor and programme director at Thrive, an NGO providing mental health services in Acholi sub-region says there is need to sensitise community members to demystify the common beliefs on causes of mental illness.
“Sensitization will prove to the community that mental illness has causes that are far from witchcraft, and there are conventional medicines to cure it,” Alal says.
Few psychiatrists
Uganda has a National Policy for Mental Health, Neurological and Substance Abuse Services, last revised in April 2010. It aims to improve access to primary care services supported by good-quality referral systems, as well as making psycho-social rehabilitation services available in communities.
But Alal says managing mental health in the region remains a challenge because there are very few psychiatrists. For example, according to Alal, only one psychiatric nurse works at the main health center IV which serves at least four sub-counties.
“Majority of people in the villages are too poor to afford transport to the health centre to seek medication. In addition, with just one psychiatric nurse at the health centre, many patients are forced to go back home without getting the medicines required,” she says, adding: “In most cases, the drugs expire because there is only one person serving hundreds of patients.”
Statistics
A 2014 study by Mental Disability Advocacy Centre titled ‘Psychiatric Hospitals in Uganda, A human Rights Intervention’, notes that the stigma of mental illness often went unchallenged in Uganda, making the recruitment of committed and educated staff particularly difficult.
WHO identified factors influencing mental health needs and services in the country, for instance the emigration of skilled medical workers, and poverty among others.
The records at the mental unit indicate that the facility receives between 1,000-1,500 patients with mental illness annually. Majority are diagnosed with Bipolar disorder, depression, substance abuse and epilepsy.