HIV patients swap ARVs for alcohol

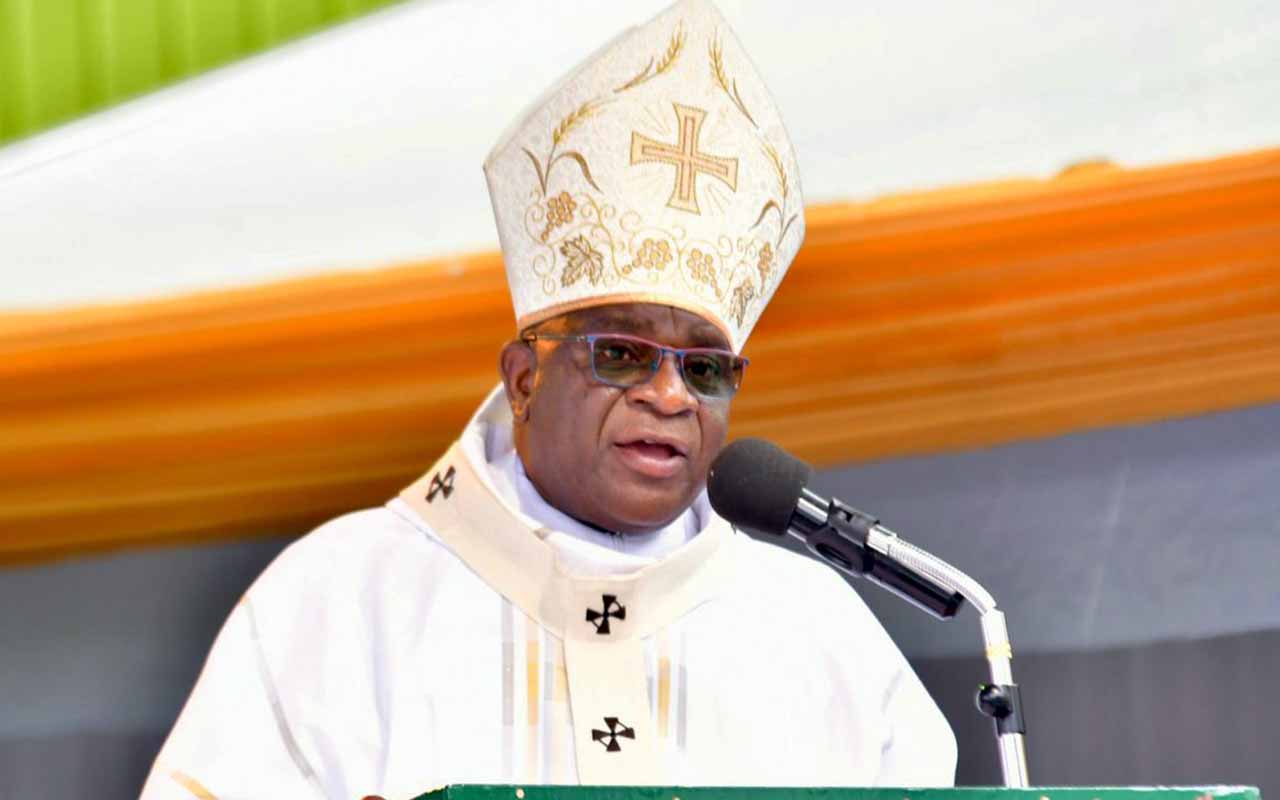
Relief. Health workers pack drugs at Amach Health Centre in Lira District recently. PHOTO BY BILL OKETCH.
What you need to know:
Stigma. Those who offer alcohol in exchange for ARVs are rich people who are also HIV positive but fear to go to health facilities to pick their drugs because of stigma.
Lira. Mr Polycarp Okello, a 25-year-old HIV patient was enrolled on life prolonging anti-retroviral (ARV) drugs six months ago.
A resident of Ewal Parish, Ngetta Sub-county in Lira District, he is aware that the anti-retroviral therapy, which has been one of the biggest successes in the fight against HIV do not cure HIV virus, but when taken promptly as directed by the doctor, they can prevent the multiplication of the virus.
Today, Mr Okello hires a boda-boda at a cost of Shs4, 000 and rides to Lira Regional Referral Hospital where he picks his share of the drugs every after two months.
He is among the 30,000 people who have been enrolled on ARVs in Lira District.
When taken properly, ARVs are part of a life-prolonging treatment for HIV patients.
“At one point, I missed taking my drugs because when I went to the hospital, I was told there were no drugs,” Okello reminisces.
“It is quite appalling when someone moves to the hospital and finds that there are no drugs because they advise us to take our drugs daily,” he says
Abuse of drugs
However, Lira District leadership notes that while the drugs benefit a big number of those enrolled on ARVs, the therapy’s abuse is threatening to turn an HIV success story into a health crisis.
“There are people who are given ARVs but when they get these drugs, and because they drink, they go and exchange them with waragi (a local potent gin),” the district acting secretary for health, Mr Anthony Ojuka, says.
Those who offer alcohol in exchange for ARVs are rich people who are also HIV positive but fear to go to health facilities to pick their drugs because of stigma.
One of the HIV/Aids patients who does not want to be named for fear of stigmatisation, says poverty is forcing them to exchange ARVs with alcohol.
“Sometimes we want to kill this stress and we do not have enough money to buy alcohol. We decide to give away the drugs,” he says.
For the infected like Mr Okello, anti-retroviral drugs are the only things standing between life and a painful death.
“There are people who have given up on life. I have buried three HIV positive people who were exchanging drugs with alcohol. Of course they died in the last four months,” Mr Ojuka says.
Aids claimed a million lives in 2016, almost half the 2015 toll that marked the peak of the deadly epidemic, a UN report said last Thursday, proclaiming “the scales have tipped”.
However, in Lango sub-region of northern Uganda, when the infected person passes on, relatives often fail to notify the facility where the victim was receiving the specialised care and treatment from.
This is where people use the opportunity to abuse the drugs left behind by the HIV patient, says Lira District health official, Ben Okao Abor.
Side effects
Mr Edmond Aceka, the assistant district health officer (DHO) of Lira, says many people fear treatment because of the side effects while others are just taken up by “circumstances whereby they don’t bother”.
“They feel the time for them to take the medicine has already passed. And some have their own lifestyles,” he explains.
“The worst case is a situation where somebody does not want people to know that he is sick and is getting medicine from far. Like Alebtong people come and get their medicines from Lira. From Lira here, there are some who are getting from Kampala and Gulu.”
And because of stigma, many skip taking their medication.
“Because if your drug is finished today and you don’t have transport means to go and pick them, it means you are going to miss for some days,” Mr Aceka explains.
Dr Florence Ocen, an HIV/Aids specialist, explained that skipping treatment has negative impact on a patient.
According to her, the lifesaving treatment is to check the multiplication of HIV virus at different levels.
“Meaning if you are supposed to take it like after every 12 hours, it means after the 12 hours the blood is without that drug,” she says.
“So if one does not really strictly follow time for taking the ARVs, you give opportunity for the viruses to multiply and they become resistant,” she adds.
The chairperson of persons living with HIV/Aids in Lira, Mr Fred Omara, says their clients are first counselled before they are introduced to treatment.
He also dismisses claims that the district has been experiencing HIV/Aids drug stock out.
“The challenge we are facing is always during the period when there is food shortage. With ARVs, it is recommended that you first eat and take it. So when the clients take the drugs without eating enough food, they get a lot of problems at night. They feel so dizzy,” Mr Omara explains.
Imat Grace takes her drugs at 8am and 8pm daily.
“I prepare tea and take with a piece of bread or cassava,” she says.
Another patient Dick Okello has been on medication since 2008.
“I’ve never experienced any difficulty in taking my drugs since I own it. I take the drugs at 6am when I am going to my work and at 6pm when I am back from work,” Mr Okello says.
Fear of stigma
The most stressing challenge in the fight against HIV/Aids is where men do not want their wives or children to know their status.
The challenge cuts across the entire eight districts of Lango: Amolatar, Lira, Oyam, Kole, Apac, Otuke, Alebtong and Dokolo.
“A man would not be interested in picking the drugs from the health facility but he would expect the wife to go and pick. Subsequently, they would begin struggling for the same drugs,” Mr Aceka says.
To battle stigma in Lira, there are plans to reward those who will come out openly to declare their HIV status.
“Whatever opportunity like relief aid, we should be giving it out to those who have come out openly,” Mr Ojuka says.
He acknowledges that many people still do not want to declare their status.
“HIV/Aids is like money. Sometimes when you ask somebody, do you have money? Nobody will tell you they have money, just like HIV/Aids,” Mr Ojuka says.
Records
In 2015, an estimated 1.5 million people were living with HIV, and an estimated 28,000 Ugandans died of Aids-related illnesses, according to Avert, a global organisation that focuses on people with HIV/Aids.
As of 2015, the estimated HIV prevalence among adults (aged 15 to 49) stood at 7.1 per cent. The number of new HIV infections in Uganda increased by 21 per cent between 2005 and 2013.
However, infections are now reducing and fell from 147,000 in 2013 to 83,000 in 2015.
In Lira, HIV epidemic has remained a big health problem.
Mr Aber says those who were HIV free are now getting infected daily.
“If you want to prove that it’s a very big thing, just sample any test carried out from any part of the district. Out of 100 people tested, you may realise even 60 have turned out to be HIV positive,” Mr Ojuka, who also doubles as the production, marketing and natural resources secretary says.
“And I think if we don’t plan well in time to come, the economy of our region will dwindle because many people after realising that they are now positive, they do not concentrate in meaningful production.”
Mr Aceka attributes the high infection rate to poverty and a breakdown in tradition and social fabric.
As of 2011, the estimated HIV prevalence among adults (aged 15 to 49) in Lira stood at 9 per cent. Seven out of 100 pregnant mothers who went for testing at health centres around the same period turned out to be positive.
According to the recently released Uganda Demographic and Health Survey 2016, about 47 per cent of men aged between 15 and 49 had ever tested and received their HIV status results in the last 12 months compared to 55 per cent of the women.
Way forward
The Ministry of Health is considering introducing an oral HIV self-test kit it hopes will prompt men to establish their HIV/Aids status.
Lira District is currently offering a number of services to HIV patients including family planning, HIV testing and counselling, safe male circumcision and provision of condoms, among others.
With concern over limited follow up of patients, ARV abuse is threatening to turn an HIV success story into a health crisis in Lira.
Issues at hand
Deaths. In 2015, an estimated 1.5 million people were living with HIV, and an estimated 28,000 Ugandans died of Aids-related illnesses, according to Avert, a global organisation that focuses on people with HIV/Aids.
Prevalence. As of 2015, the estimated HIV prevalence among adults (aged 15 to 49) stood at 7.1 per cent. The number of new HIV infections in Uganda increased by 21 per cent between 2005 and 2013.
New infections. New infections are now reducing and fell from 147,000 in 2013 to 83,000 in 2015.
Mothers. Seven out of 100 pregnant mothers who went for testing at health centres in 2011 turned out to be positive.
Testing. According to the recently released Uganda Demographic and Health Survey 2016, about 47 per cent of men aged between 15 and 49 had ever tested and received their HIV status results in the last 12 months compared to 55 per cent of the women.
Stigma. The most stressing challenge in the fight against HIV/Aids is deep-rooted in homes, where men do not want their wives or children to know their status.
Voices
“There are people who are given ARVs but when they get these drugs, and because they drink, they go and exchange them with waragi at the brewing points.” Mr Anthony Ojuka, the district acting secretary for health.
“So if one does not really strictly follow time for taking the ARVs, you give opportunity for the viruses to multiply and they become resistant,” Dr Florence Ocen, an HIV/Aids specialist.