Residents raise alarm over dirty water

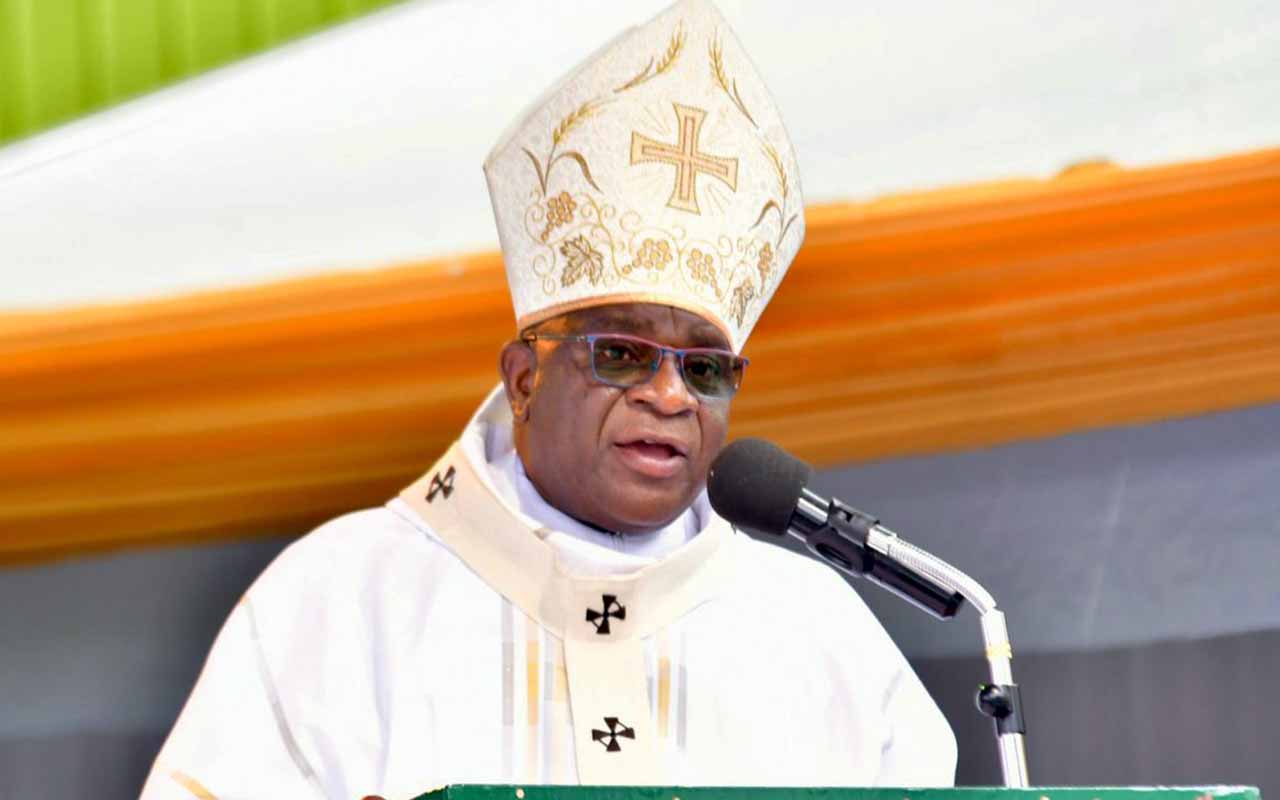
Simon Byamukama pours water into the kettle before boiling it. PHOTO BY MOSES MUWULYA
What you need to know:
- Coverage. According to Water Aid, an international organisation, eight million people in Uganda do not have access to safe water.
- Illnesses. Statistics from the district health department, the 2015/16 causes of morbidity in both adults and children below five years, were as a result of waterborne infections.
This was second to malaria, accounting for 8,087(9 per cent), followed by acute diarrhoea with 7,059 cases (10.7 per cent) while typhoid fever contributed 3,487 (2.2 per cent) cases. - Deaths. More than 45000 children under five years die due to diarrheal diseases caused by poor water and sanitation. It further reveals that about 32 million Ugandans lack access to adequate sanitation.
- Waste management. In urban areas, large slums exist without proper drainage or toilets, leaving waste to gather in and around people’s homes.
- Poverty. Without access to safe water, Uganda’s many farmers struggle to grow crops or earn a living.
There are also many nomadic communities who are difficult to reach, posing service delivery challenges. The lack of clean water and safe sanitation traps them in poverty.
Risk. - With such financial, geographical and technological challenges, Mr Dan Tayebwa, the assistant district water officer, projects that the district’s safe water coverage could shrink further.
Sembabule. Access to safe water has remained a big challenge in several parts of Sembabule District.
Most residents use dirty water for domestic purposes, exposing them to waterborne diseases. It is common to see children drawing water from ponds by the roadside for home use.
To a visitor who is not familiar with the water problem in the district, it is difficult to imagine such water can be used for drinking and cooking.
During a visit to Kabulangiti, one of the most affected villages, this reporter came across a young boy, Simon Byamukama, 10, drawing water from a pond, about one kilometre from Sembabule town.
Byamukama says they use the water much as they know it is unsafe.
“It changes the food colour. Even when we boil it for drinking, it doesn’t change much,” he says.
With a population of about 270,000 people, Sembabule’s safe water coverage stands at 36.7 per cent, which is below the national rural safe water level of 70 per cent, according to statistics from Ministry of Water and Environment.
The water problem in Sembabule is not unique to Kabulangiti Village. A tour of Ntusi, Lugusulu and Lwebitakuli sub-counties exposes the extent to which lack of clean water puts the lives of residents at risk of diseases.
Sharing with animals
Sights of people drawing water from unprotected water sources, especially from dams which they share with animals, are common. Piped water can only be found in Sembabule town.
Mr Ronald Lule, the Sembabule District water officer, explains that the change of food colour is caused by the chemical composition of the water. He adds that when one adds salt in the food, the colour is bound to change. He also says sometimes the taste of food changes. Mr Lule explains that the water can be made safer by using water purifiers. However, most of the locals do not use the purifiers because they cannot afford or access them.
“We hear of such purifiers, but we cannot afford them on a regular basis. We have no choice but to use it water without purification,” Ms Alice Namugerwa, Kabulangiti resident, says.
Ms Allen Kobusingye, another resident, says the district leadership ought to provide them with water purifiers since it is government’s obligation to provide safe water.
“With our poor financial status, we cannot afford such. Maybe our leaders would help us. But because they also do not mind about us, we leave everything to God,” Ms Kobusingye laments.
Mr Lule, however, notes that purifying water to change the chemical composition is expensive and the local government cannot afford it. He says the district has a general water problem that goes beyond the safety of the available water.
He says in some sub-counties, safe water coverage is as low as 22 per cent. In Lugusuulu Sub-county, for instance, coverage stands far below the district figure. He says Sembabule receives an average of 1,200mm of rainfall annually.
The entire district has no potential for spring wells, except Mateete Sub-county that can sustain shallow wells. For instance, Mr Lule explains, out of 190 shallow wells in the district, 170 are in Mateete Sub-county.
In such disadvantaged areas, the only alternative would be rainwater harvesting using water tanks. However, this, according to Mr Lule, is an expensive venture which many people cannot afford.
He says boreholes would have solved the problem in areas with acute water problems but the water table does not favour boreholes.
“You can drill more than 400m and you don’t hit any water-forming rock. You only drill sand which leaves the greater part of the district underserved with safe water,” Mr Lule says.
This explains why there is persistent shortage of safe water in the district, which affects sanitation and other sectors such as health; leading to waterborne infections as Mr Wilson Ssebugwawo, the district health inspector notes.
He adds: “Diseases like diarrhoea, typhoid and dysentery have continued to affect our people, mostly those in the underserved areas where people share water sources with animals.”
Statistics from the district health department, the 2015/16 causes of morbidity in both adults and children below five years, were as a result of waterborne infections. This was second to malaria, accounting for 8,087(9 per cent), followed by acute diarrhoea with 7,059 cases (10.7 per cent) while typhoid fever contributed 3,487 (2.2 per cent) cases.
Mr Sebugwawo believes the numbers may be even higher if all those who fall sick seek medical care. He notes that while the district has a sanitation grant to sensitise communities through experiments on how faecal matter contaminates water, which the natives use, and later get infected with waterborne diseases, the amount of Shs2 million annually is insufficient.
This forces them to carry out sensitisation in just a few villages, yet he says the campaign would be of a great impact.
Water tanks
Mr Lule says the district builds tanks at institutional and community level, mainly at schools and health centres, but such tanks serve a small population and for a short time before they get dry.
For this, the district receives Shs672m annually, but he says this amount is not enough because they need Shs8m and Shs3m to build a 50-cubic and 30-cubic metre tank, respectively.
“In Sembabule, you invest Shs18m and serve about six people because in three months, the water tank would be dry, assuming each person uses 20 litres of water daily,” Mr Lule notes.
Water tanks are more expensive compared to boreholes which takes Shs14 million and serves a bigger population and for a long period of time, but because of the poor water table the option for bore holes in hardly possible.
With such financial, geographical and technological challenges, Mr Dan Tayebwa, the assistant district water officer, projects that the district’s safe water coverage could shrink further.
pit latrines
Worse still, some of the leaders who would help sensitise locals do not have pit-latrines which further complicates the problem.
“It is ridiculous that some of our local leaders do not have pit-latrines. You find that almost half of the Local Council one executive in some villages do not have these facilities,” Mr Sebugwawo says, adding that they therefore have no moral authority to promote hygiene among their people. This means the water is further contaminated with faecal matter during rainy seasons as it flows to the water bodies locals draw water from for domestic use.
The district’s latrine coverage stands at around 40 per cent, which is below the national average coverage of about 68 per cent (about seven homes out of every 10), according to Uganda Bureau of Statistics.
A World Bank report released in 2012 indicated that Uganda loses up to Shs390 billion annually due to costs related to poor sanitation. The report also noted that at least 3.2 million Ugandans have no latrines, with many of them using open space to ease themselves.