Malaria: mothers and children affected Most

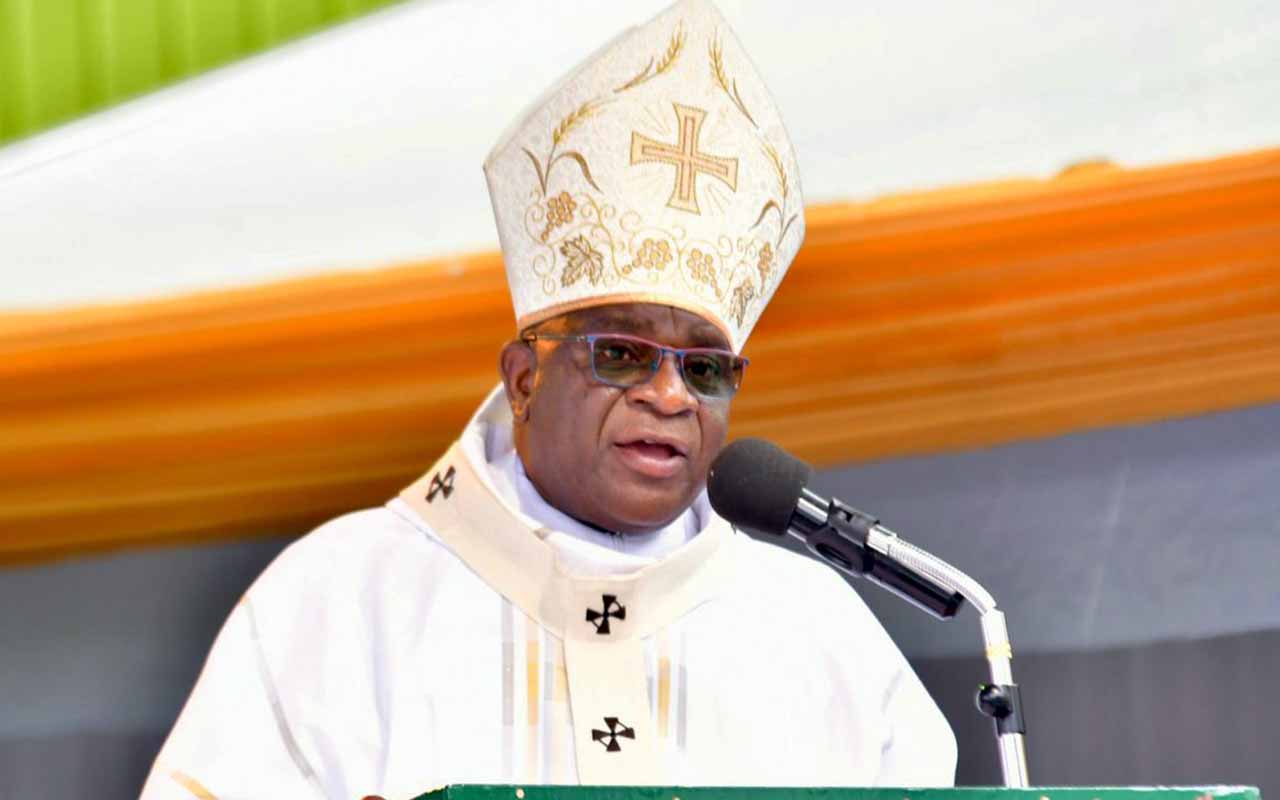
An enrolled nurse at Apac Hospital, Sister Sarah Atim treats Ms Susan Ogwara, a pregnant mother suffering from malaria. Expectant mothers and children are affected the most by the malaria burden. PHOTO BY BILL OKETCH
What you need to know:
In the last part of this series, we explore why expectant mothers and children are most affected by the malaria disease burden in Apac District.
It’s a bright morning somewhere in Owang village in Apac District, two-year-old Marion Alum is sitting on her mother’s lap at home a few kilometres away from Arocha Swamp.
Alum’s mother, Dolly Elak, 24, says her daughter has always had malaria since her birth. Currently, Alum is taking quinine syrup and paracetamol after she was diagnosed with severe malaria.
Her mother says three months ago, she was given coartem (antimalarial drug) but the fever has persisted. Alum also has diarrhoea and as I talk to her mother, she starts crying for her potty.
“I have two children and both of them sleep under a treated mosquito net. So I do not understand why Alum is always sick!” Elak says.
Alum is one of the many children in Apac District affected by the high malaria burden, which is induced by a high number of mosquito bites experienced by an individual in a night. According to the etymological infective rate (EIR) conducted in 2004, the district is known for its highest number of mosquito bites per night in the world, standing at 1,564 bites in a year with an individual suffering an average of five infectious bites a night.
Elak says she operates a road-side bar in Owang Central Parish with her husband. Owang village is separated from Apac Town Council by two huge swamps, which are believed to be safe havens for mosquito breeding.
“My daughter is now improving after she received treatment from Apac Hospital, which is about five kilometres away from here,” she adds.
However, Elak thinks that the rainy and cold weather is the cause of her daughter’s persistent fever She wonders that on top of her house being sprayed five times, her child has not had relief from fever.
“I was recently given three mosquito nets and every night I ensure that my children are properly covered under the nets,” says Elak.
Half way into the interview with Alum’s mother, another neighbour, Scovia Omara, comes to check on her. She, however, reveals that her two children were diagnosed with malaria a few days ago.
When I go to Omara’s home, her two children, Prisco Opaha aged two years and six months, is crying beside his nine year old brother, who also is on a dose of anti-malarial drugs.
Inside their grass-thatched huts, mosquito nets are very well fixed over the two beds. Omara says the children’s hut is currently leaking and has forced her to shift them to the same hut where she and her husband live.
Effects of malaria
Omara, a peasant, says her income has been totally affected by always having her children suffering from malaria.
She adds that due to poverty, she is forced to borrow money from her neighbours in order to be able to take her ill children to hospital.
The recently released Uganda Malaria Indicator Survey 2014-15 indicates that the national prevalence dropped from 42 per cent in 2009 to 19 per cent. However, Apac District continues to diagnose many malaria patients despite the northern region registering a drop from 63 per cent in 2009 to 20 per cent.
Dr Joel Ewang, a senior clinical officer at Apac Hospital, says pregnant mothers and children below five years are at a higher risk of suffering from Malaria due to their weak and low immunity given the high presence of mosquitoes.
However, Mr Ewang says due to very long experience with malaria, the native adults in Apac have developed hard immunity against malaria parasites given the many times they have suffered from the disease.
Diagnosis and treatment
Sister Sarah Atim, an enrolled midwife, found attending to two expectant mothers who have just been diagnosed with malaria, says they admit pregnant mothers at the maternity ward with various complications.
“After admission, we carry out a set of investigations according to their complications,” says Atim.
She adds: “Mosts mothers come with fever, headache and vomiting, among other issues. So after a brief talk, we send them to the laboratory.
After the laboratory tests confirming malaria, Sr Atim says mothers are immediately started on treatment to save them from getting maternal health related complications such as miscarriage, anaemia, and intra-uterine foetal death plus maternal and neonatal deaths.
Mr Geofrey Onyik, the district health educator, notes that all pregnant mothers in the district are given Fansidar during their antenatal visits to the hospital. However, the Uganda Malaria Indicator Survey 2014-15, indicates that only 25 per cent of women had the required three Fansidar doses after the first trimester.
Intervention
Dr Myers Lugemwa, the acting head of the Malaria Control Programme at the Health ministry, says through ‘Intermittent Preventive Treatment during Pregnancy (IPTp),’ a nationwide programme, mothers are advised to attend antenatal and at least have two dosages of Fansidar after three months of their pregnancy.
However, with no special attention and focus given to Apac District to counter the number of mosquito bites on the population, pregnant mothers and infants in the district will continue to suffer from malaria despite the international community hoping to have it eliminated by 2030 in the new Sustainable Development Goals (SDGs).
Why this group
Pregnant women and children are at the highest risk of malaria complications because they have low immunity. Malaria can cause spontaneous abortion, premature delivery, stillbirth and severe maternal anaemia. It is also responsible for about one third of preventable low birth weight babies.
Challenges
At Apac Hospital, malaria confirmatory tests are done through a microscope to determine whether there are malaria parasites in the patients’ blood sample. However, some local clinics still rely on the Rapid Diagnostic Test (RDT).
“RDTs are suitable for preliminary or emergency medical screening and for use in medical facilities with limited resources. They provide same-day results within two hours, typically in approximately 20 minutes,” says Dr Ewang.
Long Distance
The patients are also affected by the long distances they have to travel to get to a hospital. Susan Ogwara, 30, is one of the expectant mothers found waiting at the maternity ward. She says she didn’t know she had malaria. Ogwara explains that it all started with high fever and vomiting but due to the long distance to hospital, she didn’t have transport to go to hospital until she borrowed Shs20, 000 for boda boda.
High patient turnup
Sister Atim adds that they are also overwhelmed by the number of patients. “We struggle to attend to all the pregnant mothers coming to the ward, where one midwife attends to more than eight mothers at a time.”
She adds, “I am working alone on this shift I have to ensure that I attend to those in labour and also start malaria positive mothers on treatment as soon as I can,” Sister Atim explains her day-to-day routine.
Reporting late
Citing an example of a mother who recently got a miscarriage due to failure to report early, Sister Atim says that pregnant women always fail to go to hospital in time. She also added that those who go are not escorted by their husbands or any caretaker yet they are normally in a bad state.
“However much we give health education talks, husbands have failed to escort their wives to hospital,” Sister Atim notes.
Poverty and poor roads
She adds that most mothers who are normally referred by local health centres to come to hospital complain of lack of transport and a poor road network in the district.
No more spraying
Apac District chairman, Mr Bob Okae, says from 2008 to 2014, government deployed Indoor Residual Spraying in the district as well as in other nine districts in the mid-north to combat malaria.
However, the intervention was stopped last year yet the district continues to suffer from a high malaria burden due to the many swamps around the area which are a breeding grounds for mosquitoes.
The numbers
211
Number of paediatrics diagnosed with malaria between February and March 2015 in Apac.
9,510
Number of children between zero and four years diagnosed with malaria between February and March 2015 in Apac.
47
Number of pregnant women diagnosed with malaria between February and March 2015 in Apac.
5 per cent
Percentage of children aged zero to 59 months diagnosed with severe anemia in Apac.