Bilharzia infections hit 12m Ugandans - report

At risk. A boy plays in dirty water in Katanga, a Kampala suburb. People become infected with bilharzia when they get into contact with water in which an infected person has passed faeces or urine containing bilharzia eggs. FILE PHOTOS
What you need to know:
Treatment. Currently, there is no bilharzia treatment for children below five years. This means they are at more risk than those above five years and adults, yet they have a lot of contact with contaminated water.
Bilharzia infections in Uganda have hit 12 million cases and the threat continues, 14 years after the Health ministry launched a programme to wipe out the disease.
The ministry launched the Bilharzia Control Programme in 2003, with mass treatment of affected communities once every year with a drug called Praziquantel. The drug was used in areas with bilharzia infection of 20 per cent and above. The government also launched mass treatment of school-age children once every two years in areas where the infection ranges were from 1 per cent to 20 per cent.
However, despite its high prevalence, bilharzia is clustered among the tropical neglected diseases, with little funding allocated to combat it. This has made its control and elimination a difficult task for health experts.
A 2018 research report released by Makerere University School of Public Health indicates that 29 per cent of 40 million Ugandans are infected by bilharzia, which translates into about 12 million people suffering from the disease. The research findings say the burden is up to 42 per cent among children aged between two and four, posing a huge risk to their health.
Currently, there is no bilharzia treatment for children below five years. This means they are at more risk than those above five years and adults, yet they have a lot of contact with contaminated water.
In an earlier interview with Daily Monitor, Mr Moses Adriko, the programme officer for vector control at the Vector Control Division of Ministry of Health, said the bilharzia problem is huge yet the disease falls under the neglected tropical disease category.

Boy with Bilhazia
For years, bilharzia and other neglected tropical diseases have not been prioritised under the Health ministry budget and, therefore, receive little or no funding. Even the current drugs being administered to treat the disease are donations because government doesn’t allocate money for procurement of the drugs.
“Bilharzia is one of the serious neglected public health concerns in the country and currently, it is common in 82 districts, which have this disease as a public health concern,” Mr Adriko said.
He said while the current figures of those infected stand at about 12 million people, up to 17 million Ugandans are at risk of contracting the disease.

Transmission. A farmer cultivates his land ahead of the planting season in Butaleja District. Bilharzia infection occurs when the young bilharzia worms (cercariae) in the water penetrate human skin and enter the blood stream.
Prevalence of Bilharzia in Uganda
The latest research findings put the prevalence rate at 12 million people, representing 29 per cent of the population.
Despite 14 years of intervention, the disease burden has spread to more districts, especially along Lake Albert and those along or within islands on Lake Victoria. They include: Nebbi, Hoima, Buliisa, Kibale and Ntoroko within the Albertine region; and Mayuge, Namayingo, Buvuma and Kalangala, within or along Lake Victoria.
Findings of the survey by Makerere University School of Public Health indicate high prevalence of infection along Albertine region. Besides, individuals with severely damaged organs (spleen and liver), a condition associated with advanced bilharzia disease, have been diagnosed in fishing communities along Lake Albert and Albert Nile shores and banks, respectively.
The survey quotes reports from various health facilities indicating that some patients infected with bilharzia vomited blood during the research period.
Ministry of Health officials say in Hoima, initially this condition was suspected to be due to haemorrhagic fever or Hepatitis infections but was later confirmed to be bilharzia.
Mr Adriko said the observed increase in bilharzia infections, especially along Albertine area, is due to people’s reluctance to take medication.
“Many people refuse to take drugs because of fear of side effects; cultural and/or religious beliefs that interfere with drug uptake. There is also inadequate or total lack of sanitation leading to defecation near or within the lakes, resulting in high reinfection rates,” Mr Adriko said.
He also blamed the increase of the disease to high human-water contacts, risky fishing and snail collection practices, especially along Lake Albert.
Other factors include migration of infected people across the borders (especially from DRC), lack of safe water, highly efficient snail vectors in these areas, compounded with lack of environmentally friendly snail control measures.
What needs to be done
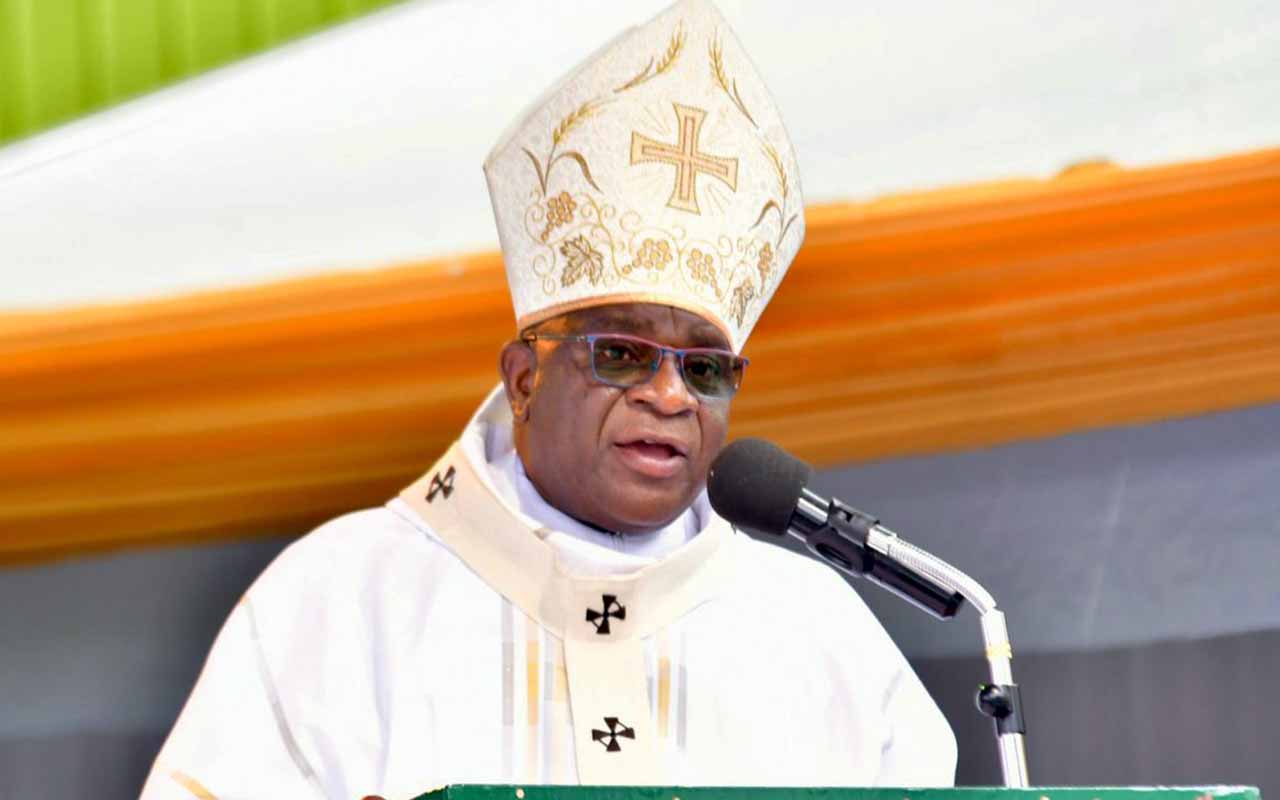
Dr Ruth Jane Aceng, the Minister of Health, says while the burden is high, efforts are being made to control the disease. She says currently, the ministry has embarked on a research on the elimination of snails without destroying the aquatic habitat.
“True, bilharzia is one of our neglected tropical diseases targeted for control because we still need more research to inform us to get rid of it without disturbing the aquatic life in our water bodies,” she says.
She says it is possible to reduce the burden of bilharzia and even eliminate its transmission in Uganda.
The minister says this requires multi-sector input from all players to be able to provide safe water supplies, mobilise communities to increase proper disposal of faecal material through use of latrines, avoiding open air defecation, increased medicine uptake during mass drug administration and control of snails in water bodies.
According to the minister, mass drug administration has had positive impact in reducing the deaths, but more must be done.
“One of the interventions we have in place is mass drug distribution in all the affected districts that surround the lakes because all our water bodies have bilharzia. The districts are given Praziquantel medicine on annual basis and because of this, deaths have reduced,” she says.
She adds that the target is both the adults and school-age children living in highly endemic areas.
Dr Aceng says while funding for the prevention and control of bilharzia has been a challenge, some resources are being mobilised to eliminate the disease.
“While it is true that funding towards this is still limited, it is not entirely true that there is no money allocated to it. When you compute all the costs of medicine, facilitating the village health workers and a number of other things, the costs come to about $3m (Shs11b). What we need to do majorly to start making progress is to get the worms out of the snails or getting rid of the snails,” she said.
She says the ministry is already mobilising funds to implement a radical plan that has been developed to eliminate the disease.
According to information from the ministry, mapping bilharzia distribution in the country has already been completed and the control programme was scaled up to all known affected districts.
Districts with high prevalence are targeted for bilharzia control and mass treatment is given once every year. Districts with low infection rates are targeted for elimination of bilharzia and are treated once every two years. Currently, 82 endemic districts, with a population of 17.9 million people at risk of infection, are being treated.
Any success?
The Health ministry says more than 26 million people have been treated of the disease over the years. Community awareness about causes and preventive measures for bilharzia has increased significantly in some districts. The ministry says some districts have made great strides in eliminating the disease.
In some districts such as Amolatar, Gulu, Kabarole, Moyo, Mpigi, Nakasongola, Dokolo and Mubende, infection has been reduced from above 70 per cent to less than 20 per cent.
The Health ministry says the treatment strategy in some of these districts has been changed from once annually to once in two years. Similarly, in these districts, the proportion of those with affected organs due to bilharzia has reduced from 40 per cent to below 6 per cent.
Cause
Bilharzia is a water-borne disease caused by parasitic worms or flukes called schistosomes. These are found in blood vessels of infected people. There are two forms of bilharzia: the intestinal and urinary types. Intestinal bilharzia is where adult parasite worms live within blood vessels around the intestines of an infected person, while urinary bilharzia is where the adult worms are found in blood vessels around the urinary bladder.
Transmission
Transmission occurs when an infected person passes faeces or urine containing bilharzia eggs in or near fresh water bodies. When the eggs reach water, they hatch into larva. The young larva penetrate specific types of freshwater snails commonly found in water bodies.
Within the snail, the young worms grow, multiply and develop into a stage of young worms called cercariae, which can infect human beings. The young worms emerge from the snails in large numbers into the water and swim in the water looking for a human host.

How Bilhazia is transmitted
People become infected with bilharzia when they get into contact with such water while fishing, swimming/playing, bathing, fetching water, washing clothes, wadding and cultivating in swamps.
Infection occurs when the young bilharzia worms (cercariae) in the water penetrate human skin and enter the blood stream. Thus, bilharzia occurs in places where communities living near water bodies pass urine and stool in the water sources.
The disease presents with persistent abdominal pain, bloody diarrhoea or urine, general body weakness, anaemia and fever.
At late or chronic stage, bilharzia can lead to retarded growth; weight loss and enlarged spleen and or liver. Enlarged organs may lead to accumulation of fluids into the abdomen resulting into a very swollen, distended abdomen. Bilharzia kills when an infected person grows a swollen abdomen and starts vomiting blood. In its late stages, bilharzia is irreversible and leads to death.
Background
Most affected districts. Despite 14 years of intervention, the disease burden has spread to more districts, especially along Lake Albert and those along or within islands on Lake Victoria. They include: Nebbi, Hoima, Buliisa, Kibale and Ntoroko within the Albertine region; and Mayuge, Namayingo, Buvuma and Kalangala, within or along Lake Victoria.
On treatment. Currently, 82 endemic districts, with a population of 17.9 million people at risk of infection, are being treated.
Some success. In some districts such as Amolatar, Gulu, Kabarole, Moyo, Mpigi, Nakasongola, Dokolo and Mubende, infection has been reduced from above 70 per cent to less than 20 per cent.