Inadequate protective gear frustrating Covid-19 fight

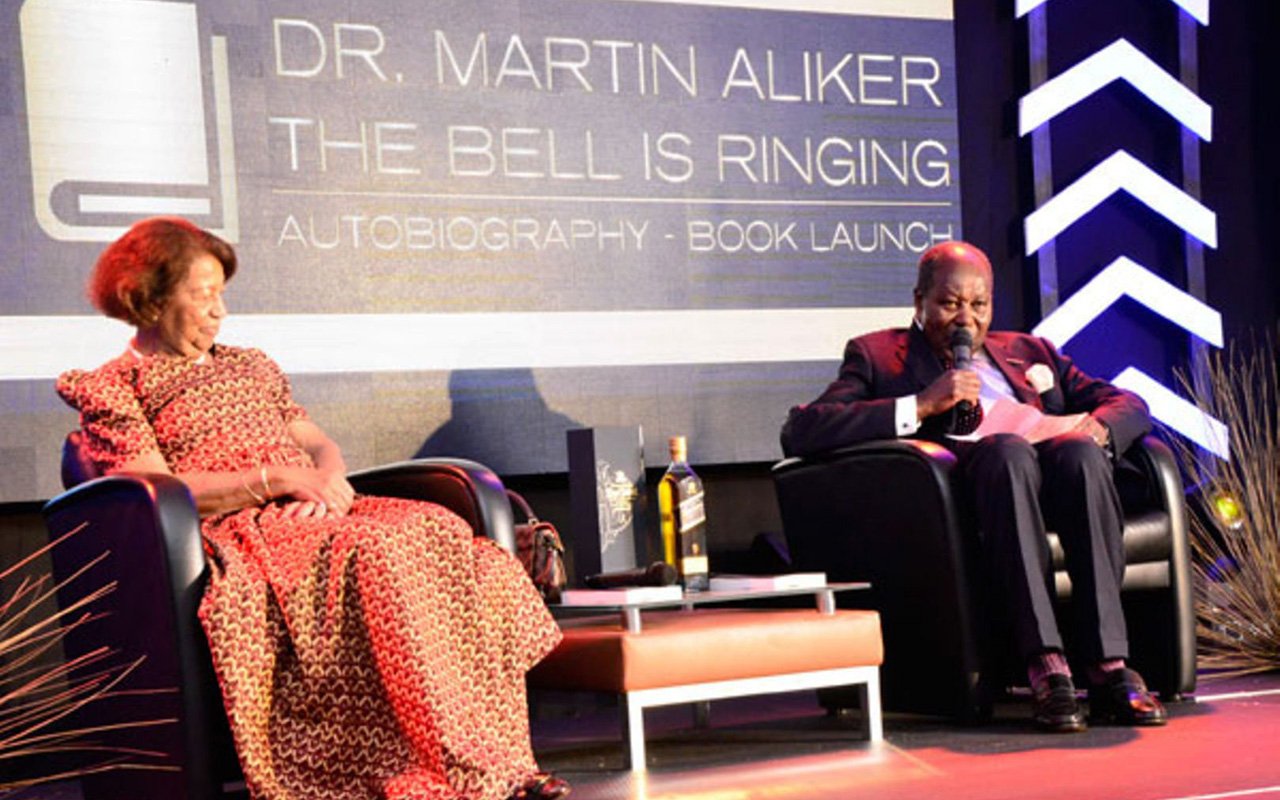
Protected. Health workers at Mulago Specialised Hospital see off seven patients who recovered from coronavirus on March 18. Many health workers say they do not have enough personal protective gear. PHOTO BY RACHEL MABALA
What you need to know:
- Protection: Whereas the Health ministry has been recommending the use of personal protective equipment since the outbreak of Covid-19, little has been done to ensure this is achieved, especially by those on on the frontline against the disease, writes Isaac Mufumba.
On Monday, health workers at Princess Diana Health Centre IV in Soroti District, went on strike protesting failure by the authorities there to provide them with personal protective equipment (PPE). The nurses had by Thursday morning not returned to the wards.
Dr Alfred Anyonga, who heads the facility, said supply of masks and gloves has been perpetually inadequate, adding that they have been mostly making do with “borrowed” masks and gloves from The Aids Support Organisation (Taso) and the Covid-19 quarantine centre at the nurses’ training school.
“We have been receiving an average of 20 pieces of masks weekly from the district health office against 34 staffs working on daily basis. We would borrow some to bridge the gap, but the time is so difficult that they can give us no more,” Dr Anyonga said.
However, the Soroti Town Clerk, Mr Moses Otimong, says the industrial action is not about only lack of PPEs.
“I was served with notice from the facility raising matters of delayed payment of coronavirus risk allowances for the deployed staff,” he said.
Elsewhere
As Mr Otimong addressed Saturday Monitor in Soroti, about 30 nurses at Jinja hospital were demonstrating in protest of delayed payment of their risk allowances. The nurses claimed that their allowances had not been paid since they were first deployed in March.
The Soroti Resident District Commissioner (RDC), Mr William Wilberforce Tukei, says delayed payment of allowances and lack of PPEs is not peculiar to Princess Diana Health Centre IV, but to all facilities in the district, if not the whole country.
It would now appear that Uganda’s response to the outbreak of the Covid-19 pandemic is being hampered by lack of access to personal protective equipment such as gloves, medical masks, goggles, face shields, gowns and aprons, among others.
Since the outbreak of the pandemic, the Ministry of Health has been disseminating information on the use of PPEs at various levels. The ministry recommends the use of N95 masks in Covid-19 isolation centres and by those working in laboratories or taking samples.
The Uganda Medical Stories (UMS) is expected to provide the PPEs, but it appears the institution has fallen short.
On Wednesday last week, the Uganda Medical Association (UMA) issued a press statement pointing out that despite the huge government budget allocation and equally huge amounts in donations channelled towards the purchase of PPEs, 13 out of its 14 branches in the country had reported stockouts and inadequate supplies of the same.
According to a statement that the Minister of Health, Dr Jane Ruth Aceng, issued in Parliament on April 7, the biggest percentage of the government’s budget for the Covid-19 response is aimed at catering for logistics, especially PPEs and laboratory testing kits for six months’ supply. That was to take up Shs176.6 billion.
According to the statement issued by the UMA secretary general, Dr Mukuzi Muhereza, the shortages are unacceptable.
“The Occupational Health and Safety policy and guidelines provides for the protection of the health worker from potential risks such as Covid-19 through use of adequate PPEs. The world over, we have seen that thousands of health workers have been infected with Covid-19 and with limited or no PPEs, the risk is enormous. This is completely unacceptable to risk the lives of the frontline health workers,” the UMA statement reads in part.
Whereas there are indications that there has either been no community transmission or that if there are any cases of coronavirus in the communities they are of low severity, health workers are not taking any chances.
The president of the Uganda Nurses and Midwives Union, Mr Justus Cherop Kiplagat, says whereas government has been providing some PPEs, most of the health workers have been using their own money to procure PPEs to protect themselves from being infected and possibly infecting others.
“Some protective gear has been provided, but they are simply not enough. Each medic is provided with, for example, only one facemask. You take it off and clean it, but before it dries, another patient comes in for treatment. Each medical worker should have at least two pairs of masks,” Mr Kiplagat says.
He says the situation needs to be addressed if Uganda’s Covid-19 response is to be successful.
“If any nurse or doctor get infected, it means very many more people will get infected. That is why it is critical that this is treated with utmost urgency,” Mr Kiplagat says.
The reports of the shortages are occurring shortly after Parliament passed a supplementary budget which provided the health sector with an additional Shs404b to support Uganda’s response to the pandemic.
Under the supplementary budget, Shs54b was made available to cater for purchase of 38 ambulances, personal protective equipment, beds under Intensive Care Units (ICUs); ventilators and provision of oxygen plants in the national referral hospitals, and regional referral hospitals.
Shs50b was provided to cater for salary of staff to be hired on contract to bolster staffing levels; allowances for staff on surveillance; accommodation for those under quarantine; provision of blood; and provision of medical supplies, including gloves, masks and sanitisers. So why the shortages?
By press time, it was not possible to engage Dr Aceng over the shortages or performance of the Covid-19 budget so far.
However, in a statement she issued on Thursday last week, the minister indicated that government had not been able to mobilise all the funds needed for the Covid-19 response.
“To date, the government of Uganda has mobilised Shs314b out of Shs990b required for the health sector to support the Covid-19 response,” she pointed out.
Giving un update of what had so far been done, the minister pointed out that the capacity of the district taskforces had been bolstered by the recruitment of epidemiologists and the deployment of physicians to be based in the regions to support district and regional functions; strengthening of the regional referral hospitals to manage cases of Covid-19, and carrying out of the rapid community assessment surveys.
Dr Aceng also pointed out that the rolling out of the testing of alerts and contacts, and sample removal from district and regions; put in place a mechanism for quick identification of imported cases; enhanced risk communication and social mobilisation, and ensuring continuity of essential and routine health services.