The submissions: Death during a fibroids operation
On October 14, 2010, a patient died at the Women’s Hospital International in Kampala at the start of a surgical operation to remove fibroids from her uterus using a technique known as laparoscopic surgery.
Two pathologists who carried out a post-mortem examination of the body of the patient found half a litre of blood in the stomach of the patient.
The pathologists concluded that the patient had died due to lack of oxygen when the tube to supply oxygen to her lungs was wrongly inserted into her oesophagus instead of her trachea.
Prosecution
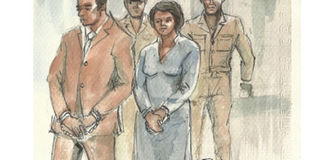
Dr Tamale Ssali the proprietor of the hospital and an anaesthetist at the hospital were prosecuted for having caused the death of the patient by a rash or negligent act. It was the sole responsibility of the State to prove beyond reasonable doubt that the two accused persons acting together did a rash and negligent act leading to the death of the patient.
Submissions of the accused
The lawyer who represented Dr Ssali implored court to acquit his client. His main grounds were that the section of the law under which his client was charged did not support the particulars of the offence.
And that a common intention between the two accused persons had not been proved by the State and that the doctor was never in the theatre at the time the alleged rash and negligent act. To the lawyer the State failed to put his client at the scene of crime.
The anaesthetist’s lawyer also asked court to acquit his client. He submitted to court that his client had performed his duties very well otherwise the operation would not have commenced at all and further that the chief surgeon had approved of the preparations even before the surgery.
According to the lawyer, if indeed there was wrong intubation, the 10 minutes it took the surgeon to carry out the first procedure (hysteroscopy) would have sufficed to reveal the defect.
To the lawyer the cause of death was stated as “intra-operative neurogenic cardiac arrest and associated acute gastritis” and this had nothing to do with absence of oxygen in the body.
To him, the post-mortem report was also incomplete since no toxicology or histology reports were submitted by the prosecution.
Submissions by the State
The State submitted that this case had been proved beyond reasonable doubt against the accused persons. The State told court that Dr Ssali participated in the operation that led to the death of the patient; he was clad in a green theatre gown when he approached the elder sister of the deceased twenty minutes after the patient was taken to theatre.
The doctor approached her to ask if her sister had any pre-existing conditions or a history of alcohol or drug abuse and told her to prepare for “anything”. The communication between the doctor and the sister of the patient showed that he was in theatre at the material time.
Dr Ssali pinned
The State also submitted that Dr Ssali was the primary doctor in this case and had a duty of care to the patient which duty he did not deny before court. The State told court that the facility was owned and run by Dr Ssali and this facility did not have adequate equipment for anaesthesia, for laparoscopic surgery and for resuscitating patients in case the need arose as in this case.
The fact that Dr Ssali knew that his hospital did not have these facilities but went ahead to employ the anesthetist to participant in such specialised operation showed that the two had a common intention as the two should have known that undertaking such an operation in the circumstances was very risky.
The State concluded that all the prosecution witnesses were very consistent and there were hardly any contradictions in the evidence presented, which evidence put both the accused persons at the scene of the crime.
The State implored court to dismiss the defense put up by the accused persons as a pack of lies and invited court to convict both accused persons as charged.
Observations
There was no evidence adduced to the effect that the operation had indeed commenced successfully and lasted 10 minutes and anesthesia appropriately given. The post-mortem report clearly established that the patient died at the beginning of the operation.
The State did not submit elaborately on the blood in the stomach which was at centre of this case.
The purpose of a post-mortem examination is to establish the cause of death and this may be done without investigations such as toxicology and histology. The State did not submit further on the technical terms used to state the cause of death.
The post-mortem report was a technical document and the cause of death as stated therein had technical terms but the evidence given in court clearly explained these technical terms.
The evidence from the Uganda Medical and Dental Practitioners Council gave further credence to the cause of death.
Next; the judgment




