Prime
Constraints, challenges in using insulin
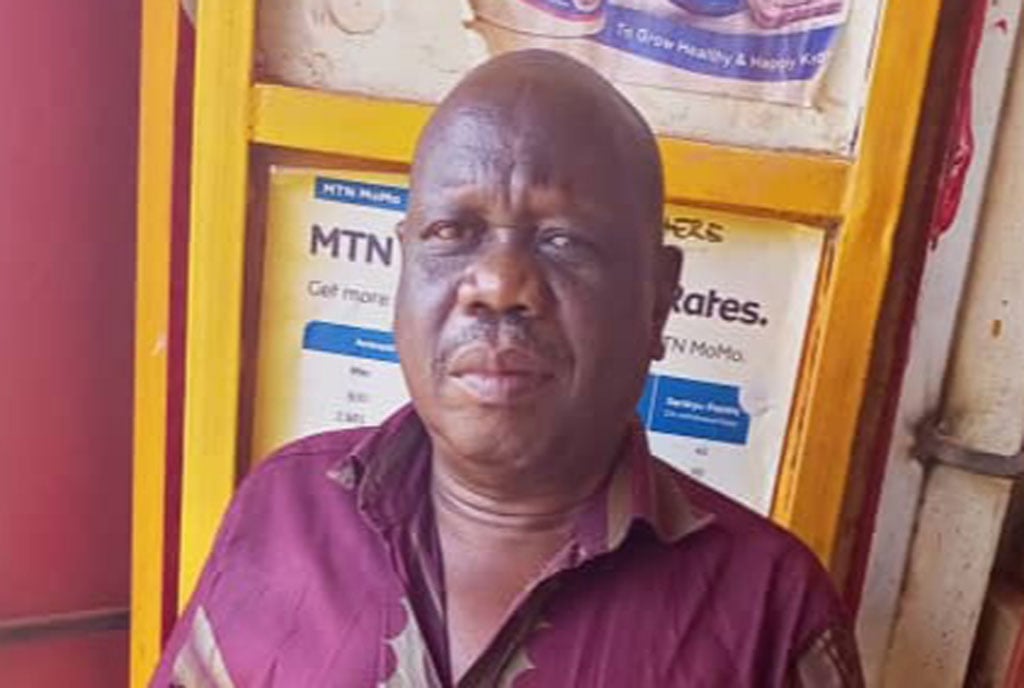
Aziz Kisolo who was diagnosed with diabetes at the age of 21. PHOTO/COURTESY
What you need to know:
- On November 14, World Diabetes Day was commemorated under the theme “Education to Protect Tomorrow”.
- We look at some of the challenges in accessing insulin in Uganda and what can be done to make it easy to access this life-saving drug.
Azizi Kisolo (64), was diagnosed with type-1 diabetes at the age of 21 and has since been on insulin. The Uganda Diabetes Association deputy secretary is, however, concerned about the exorbitant cost of treating his condition.
“I have to take insulin for the rest of my life. However, access to it and to the self-care material is expensive. I use about Shs300,000 every month on top of buying the glucometre,” he says.
According to Dr Susan Nakireka, a diabetologist at Mengo Hospital in Kampala, insulin should be free in government hospitals. However, the government has not been able to provide insulin to the people who need it and, in most cases, they have to buy it on top of the extra self-care material. This makes the treatment of the disease expensive yet most of the patients that suffer from it are not well off,” she says.
In order to take the self-injectable insulin, one needs a needle that should be disposed of after every use. However, Kisoro uses his needle 10 times before he throws it away. This, Dr Nakireka says, increases the patient’s risk of catching infections.
The global burden
Across the world, the numbers of diabetes cases are increasing rapidly, especially in low and middle-income countries. These soaring numbers are worsened by limited access to insulin, a known diabetes remedy, which is fast becoming a global crisis. About 80 percent of people with diabetes are in lower-to-middle income countries.
A report by the Access to Medicine Foundation indicates that people with diabetes in under-resourced countries are not currently getting the choice of insulins they need, and access to this life-saving drug is severely limited in many of these countries.
“While diabetes care and treatment has advanced since the discovery of insulin a century ago, this highly effective drug, and the range of products that help manage chronic diabetes, is only available to a fortunate few,” says Jayasree K. Iyer, CEO, Access to Medicine Foundation.
What is insulin?
Dr Nakireka says insulin is a naturally occurring hormone made by the pancreas, which regulates the amount of glucose in the blood. Without enough insulin, glucose builds up in your blood, causing diabetes.
There are two types of diabetes; type 1, which is more common in children and adolescents but can also occur in adulthood and is said to be caused when the body’s immune system accidentally attacks the cells in the pancreas that it stops making insulin.
“With type 2 diabetes, however, the body becomes resistant to the effects of insulin. As a result, the body overproduces insulin to keep your blood glucose levels normal. With time, this overproduction causes a burnout to the pancreas and the result is type-2 diabetes,” she says.
Diabetes cannot be cured but taking insulin or other diabetes medicines is often part of the treatment in addition to making healthy food and beverage choices, physical activity, getting enough sleep, and managing stress.
“The injectable insulin is identical to the insulin made by the body. Once one is diagnosed with type 1 diabetes, they are started on insulin immediately. People with type-2 diabetes usually start taking other medications besides insulin but when their blood sugar is not controlled, even with the medication, then they are started on insulin,” says Dr Nakireka.
How to take insulin
If your health care provider prescribes insulin, a trained diabetes educator or pharmacist will teach you the proper dosage and how to administer your daily injections. One can use a needle and syringe, an insulin pen, or an insulin pump. The needle and syringe is the commonest in Uganda because it is cheaper.
“I get my daily insulin shot using a needle and syringe. I was shown how to draw up my dose of insulin from the bottle through the needle into the syringe then inject it into the belly,” says Kisolo.
Some people with diabetes need two to four shots a day to reach their blood glucose targets and Dr Nakireka warns against injecting insulin in the same spot repeatedly because it may harden the tissue over time, making it harder to take shots in that area. Other spots to inject insulin include the thigh, buttocks, or upper arm, although it may take longer for the insulin to work once injected in these areas.
When?
Once you are diagnosed with type 1 diabetes, the pancreas does not make any insulin so you need to start this treatment immediately. For type2 diabetes, one has trouble controlling blood glucose with diet, exercise, and other oral or non-insulin injectable diabetes medications.
If your blood glucose level is higher than 300 mg/dL at any time of day (or higher than 250 mg/dL after not eating for at least eight hours). If your body reacts to other diabetes medications and has poorly controlled blood glucose.
You often experience thirstiness, frequent urination, or other symptoms of high blood glucose despite taking other diabetes medications.
The challenges
According to Dr Nakireka, the government has made little investment when it comes to non-communicable diseases. Although healthcare is a human right, she says there is no access to some drugs.
In some health facilities, there are no testing kits and some health workers need training to get a deeper understanding of the disease.
Storage of the insulin is also a challenge, especially for people who take the shots more than once a day.

Awareness On November 14, World Diabetes Day was commemorated under the theme 'Education to Protect Tomorrow.'
According to Dr Nakireka, insulin should be stored in a cool place (a refrigerator preferably), away from sunlight.
Many people, according to Kisolo, are duped by herbalists who say patients can be cured using herbs. This, he says, has led to many of his colleagues developing complications and others dying.
“People need to understand that there is no cure,” Kisolo emphasises.
What to do
While companies’ efforts currently fall short in addressing the extent of the global insulin inequity problem, an Access To Medicine Foundation report identifies ways in which these companies are now seeking sustainable approaches to scaling up access.
Insulin manufacturers; Eli Lilly, Novo Nordisk and Sanofi have diverse strategies in place to expand access to their products. Notably, Novo Nordisk and Sanofi have recently taken steps to apply integrated business approaches encompassing some of their insulin products.
However, the report indicates that there are persistent gaps in access to all insulins; most affordability strategies remain primarily focused on human insulins and few are found for analogue products.
It is within these companies’ abilities to expand access if they build on the strategies they have already employed, with the report identifying ways in which they are now seeking sustainable approaches to scaling up access.
Breaking down the cost
● The cost of treating the disease is a very big challenge to so many people. Among the items needed for self-care is a glucometre which costs between Shs70,000 and Shs150,000.
● One needs to check their sugar levels three times a day and the strips needed for this test cost Shs1200 and Shs1500 per strip. A pricker costs Shs1000. These are used once.
● A bottle of insulin costs Shs25,000 and Shs45,000, depending on where you buy it from. One may need about two or three bottles a month. The insulin pen, which is easier to transport, is even more expensive. It costs Shs70,000 and Shs150,000 and contains only a third of what is in the bottle. It is usually refillable.
● The needles cost Shs500 but those for the insulin pen can go up to Shs1,000.




