Alcoholism, drug abuse triggers mental illness among refugees

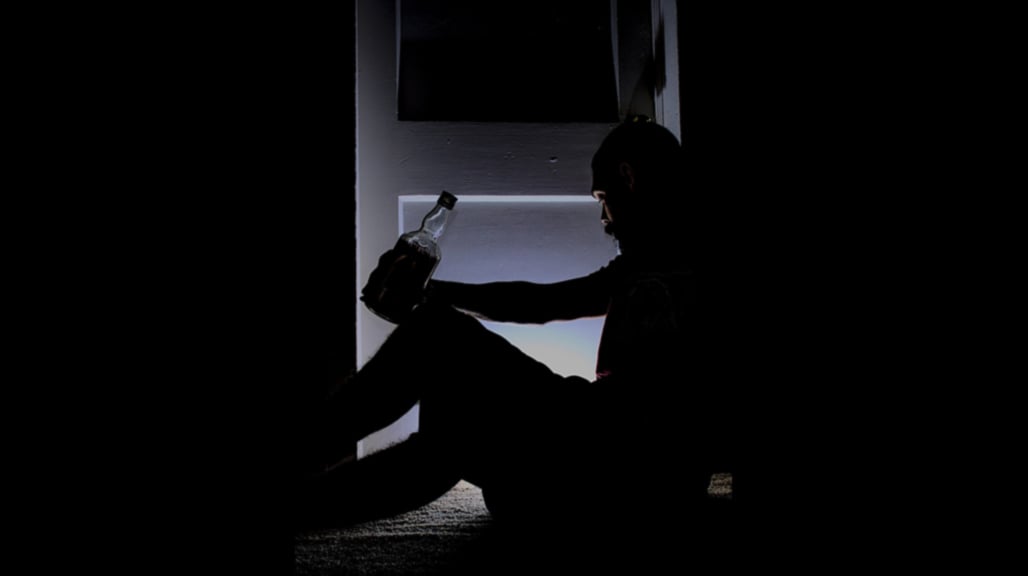
A group of youth take alcohol in Adjumani Town last year. PHOTO | MARKO TABOIT
What you need to know:
- A recent World Health Organisation study estimates that one in five people in post-conflict settings suffer from mental health problems.
A new study has revealed that the high prevalence of mental health and suicide cases among refugees in settlements in Adjumani District are caused by alcoholism and substance abuse.
The researchers sampled Nyumanzi, Boroli, Majji, and Mungula refugee settlements out of the total 19 refugee settlements in the district and interacted with refugees aged between 15 and 34 years.
“The survey revealed a 14 percent substance abuse rate among the refugees. Common substances consumed consisted of marijuana, mairungi and tobacco being the most consumed at least two-three times a day; with most chewing and smoking, respectively,” part of the report reads.
Findings also revealed that drugs consumed are shared (67 percent) among the refugees.
Alliance Forum for Development (AFOD-Uganda) published the report titled: Mental Health and Psychosocial Support (MHPSS) baseline assessment in Adjumani, in November 2021.
Mr Michael Mawa, a programmes manager at AFOD, told Daily Monitor that the goal of the research was to identify the cause of the vices in order to develop appropriate solutions.
Mr Mawa says the study established that a significant proportion (82 percent) of refugee households faced mental health issues resulting from limited or no access to basic needs such as food, illnesses, loss of personal properties, among others.
“Other factors were identified as physical body injury (34 percent refugees), gender-based violence (10 percent, especially rape cases in refugee), forms of affliction (20 percent torture) including workload, kidnap, feeling of guilt and worthless, among others,” Mr Mawa says.
Whereas mental health systems still remain weak and uncoordinated, Mr Mawa said there is no functional mental health unit to support mental health cases at the district and regional level.
“This is coupled with the limited staff capacity to provide MHPSS service. In addition, there is no or limited space provided to manage mental health patients at HCVs and district hospital,” he adds.
The researchers recommend that access to and utilisation of mental health and psychosocial services be improved by strengthening the capacity of lower community structures to identify and refer individuals for MHPSS support.
“This includes training of village health teams (VHTs) and other community volunteers to identify mental health clients and provide first-care MHPSS, and also train local leaders, including refugee welfare council leaders on aspects of mental ill-health,” the research states.
It adds: “The District Council should consider reviving local ordinances (by-laws against selling of illicit substances (alcohols and drugs) and make operational funds available for effective monitoring of such legislative by-laws.”
Mr Moses Nyang, the Refugee Welfare Council (RWC) secretary for Nymanzi Refugee Settlement, in an interview agrees with the report findings.
“One time I staged a crackdown on opium smokers and netted many of them and these vices continue every day while security (police) deployed around to watch,” he says.
He adds: “Today we have mobilised up to 40 refugee leaders where we patrol their hideouts at night and once we get them, we call the police and get them arrested.”
Mr Nyang also attributes the trend to persistent economic problems and social factors including the reduction in food ratio, triggering desperation and stress.
“Due to the economic hardships, refugee youth have formed cliques, especially in Ayilo 1, Pagirinya, and Maaji, and have resorted to excessive alcoholism, substance abuse characterised by violence, sexual harassment, among other crimes,” he says.
Despite the rapid rise in mental health problems in the district, mental health services have been neglected and grossly underfunded.
The current treatment available at Adjumani Hospital benefits very few individuals.
The Covid-19 pandemic has further exposed the gaps the mental health system has faced for a long time in the district and the region leading to increasing reported cases of GBV, suicide, and observed hopelessness.
Sr Alice Bunia, the officer-in-charge of Mental Health at Adjumani General Hospital, reveals that the district in the last two years recorded 5,000 cases of mental health and each year with about 10 cases of suicide.
Sr Bunia says they administer counselling services to suicide survivors.
A recent World Health Organisation study estimates that one in five people in post-conflict settings suffer from mental health problems.
A recent World Health Organisation study estimates that one in five people in post-conflict settings suffer from mental health problems.