Death following wrong blood transfusion - part I
On February 6, 2010, a 38-year-old mother of four breathed her last in the intensive care unit of Mulago hospital. Her youngest child was only a day old. The mother had been operated on the previous day to remove the premature baby of eight months.
A few months prior to her death, the mother, then carrying her fourth pregnancy, noticed she was having episodes of abnormal bleeding in the course of the pregnancy. She had had two previous caesarean sections. An ultrasound scan examination of the uterus revealed that the placenta in this pregnancy was lying in the lowest part of the uterus and this was the cause of the intermittent bleeding. Technically this is known as placenta previa and she had the worst type, that which was obstructing the opening of the uterus.
This, therefore, meant that of necessity she had to have caesarean section in order to deliver the baby. It is not uncommon for a placenta to lie in this position following repeated operations on the uterus; she already had two operations. The normal is for the placenta to lie in the upper part of the uterus.
Her medical care was covered by a regional insurance company. The company had a clinic that offered antenatal services but not delivery. And so in the course of the antenatal services, the mother’s blood group was determined and recorded on her antenatal card as B+.
She also had a consultant obstetrician attending to her. In January the consultant had seen her in private when she was admitted there following an episode of bleeding. The consultant also saw her on two antenatal visits to Mulago hospital.
On February 6, the patient, then five weeks to her expected date of delivery, was admitted in Mulago hospital when she had another episode of bleeding which was quite profuse. The consultant decided to carry out an emergency operation to save the baby and the mother.
However, even after the removal of the baby and offending placenta, the mother continued to bleed profusely and the surgeon had no option but to remove the patient’s uterus in an attempt to control the bleeding. And during the operation the mother needed an urgent blood transfusion. She was transfused with blood group B+ to which she subsequently reacted. The staff in Mulago hospital discovered that the patient’s blood group was O+ and not B+ as had been stated on her antenatal card.
The patient’s condition continued to deteriorate and she was transferred to the intensive care unit. It was noticed that the patient was not passing urine and later that night she was transfused with blood group O+. She passed away the following day. A postmortem carried out the following day established that the patient had suffered hypovolaemic shock, multiple organ failure and bleeding abnormalities.
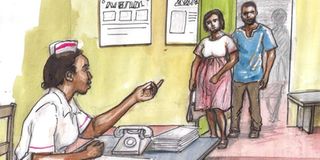
The family of the deceased sued three parties; Mulago hospital through the Attorney General, the consultant who attended to and operated on the patient and the private health care provider citing medical negligence and breach of duty of care. At centre of the suit was who was responsible for erroneously stating that the deceased was of blood group B+ when in truth she was of blood group O+. Another related issue was who bore the responsibility of the mother’s death.
Blood transfusion and its complications
Blood transfusions, often lifesaving, are not without adverse effects. A blood transfusion is a medical procedure during which blood (often from another person) is given to a patient in need of it. However, a patient must be given blood of a compatible group.
A wrong blood transfusion will lead to clumping of red blood cells and a reaction that can lead to the collapse of the circulatory system. Before each blood transfusion, the patient’s blood type must be determined and then tested against the blood to be transfused. This is known as grouping and cross-matching.
To be continued




