Prime
Botched surgery to remove uterus
What you need to know:
- This medical procedure is known as a total abdominal hysterectomy and it was explained to her that the operation entailed the removal of her uterus, which also meant that she could not bear any more children.
- She signed a consent form for the operation, having understood what the operation meant.
Ms Jonas, a 49-year-old school teacher, was diagnosed with intra-uterine fibroids in 2011.
Considering her age, the best treatment option given to her was a surgical operation to remove her entire uterus.
Total abdominal hysterectomy
This medical procedure is known as a total abdominal hysterectomy and it was explained to her that the operation entailed the removal of her uterus, which also meant that she could not bear any more children.
She signed a consent form for the operation, having understood what the operation meant.
She, however, did not read the hospital consent form that she signed; she was apparently happy with the explanation given by the doctor.
The operation
The operation was carried out on September 15, 2012 in a government hospital and Ms Jonas was discharged from hospital on September 17, 2012, two days after the surgery.
The doctor who performed the operation advised her on how to clean the wound and was also given some medication to take. She was told to visit a health facility close by her place of abode, 10 days thereafter, to have the stitches removed.
The patient, as advised, visited a local clinic on September 27, 2012 so that the stitches could be removed, which was done. At the time of removal of the stitches, the wound appeared healed.
Excruciating pain
However during the night of September 27, 2012 she started to experience excruciating pain around the pelvic area, which pain she described as surpassing labour pains. The pain was so much that she could not drive and a colleague had to drive her to a hospital close by.
While in the Accident and Emergency Department, Ms Jonas experienced the discharge of a greenish fluid from her private parts. After she was accessed in the hospital, she was referred to a higher level hospital that night.
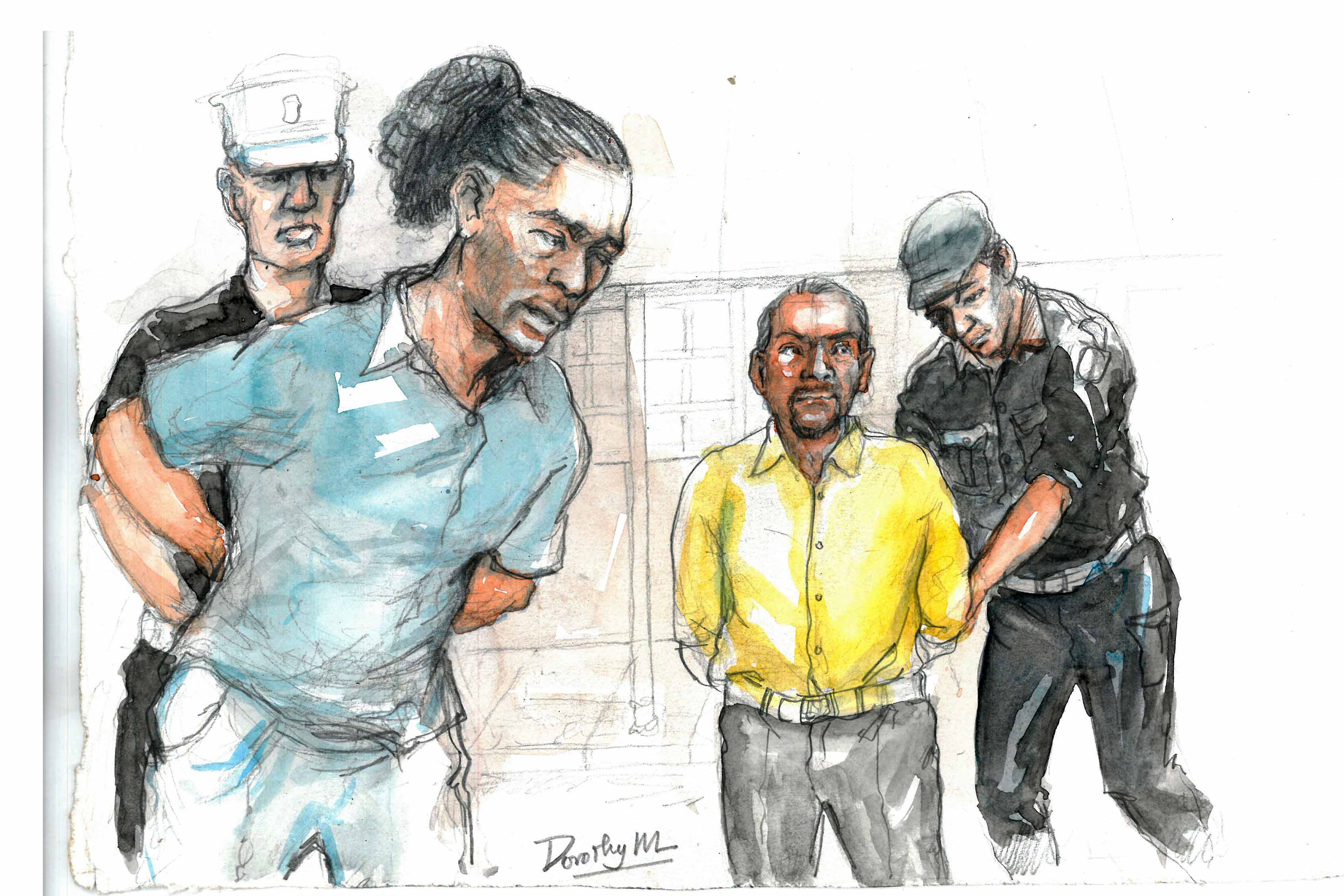
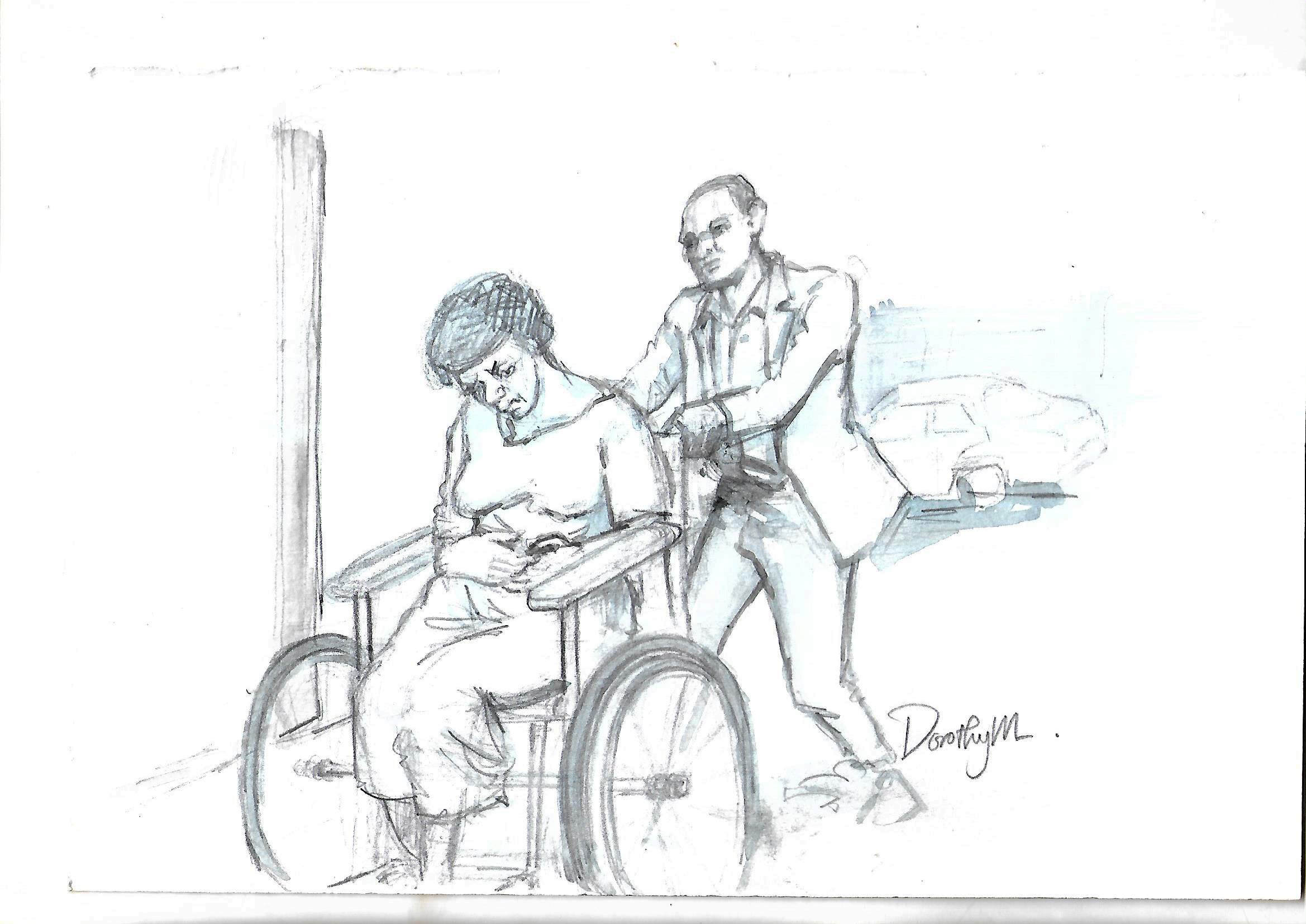
Upon her arrival at the hospital she was referred to, the unbearable pain persisted to the extent that she could not walk on her own; she had to be put on a wheelchair and rolled into the hospital.
Greenish fluid leakage
The flow of the greenish fluid intensified so much so that she had to be given heavy duty sanitary pads to put on. The doctors who attended to her, however, did not inform her about the cause of the fluid leakage, despite her persistent enquiry.
She was later told that the leakage was as a result of water collecting in the hole where the uterus had been. She was given antibiotics to treat the condition.
She was discharged from hospital on October 4, 2012 although the fluid was still leaking. She was given a supply of maternity pads in addition to the antibiotics.
Seeks second opinion
The patient sought a second opinion from a private medical facility but she was advised to go back to the hospital where the surgery was carried out from to seek further clarification about her condition and for the doctors there to manage her condition. She heeded the advice and on October 12, 2012, she returned to the hospital where she was operated from.
She was immediately admitted and a catheter was inserted into her and she was given diapers to use.
Injured ureters
It was explained to her that she was leaking urine and this was because one of her ureters had been injured at the time of the operation to remove her uterus. She was told that the leakage would eventually stop.
She was discharged and given more diapers to use. The catheter was not removed and she was told that she would need until the leakage stopped completely.
Ms Jonas was, however, greatly inconvenienced by the catheter; it dangled in between her legs. Whenever she had to sit down, she needed a blanket or cloth to it.
Isolation
At home, her husband displayed loss of affection. He would not sit next to her and at night he would sleep on the floor.
Due to the flow of urine, she developed a stench of urine and this strained her marriage. Her home caretakers were only her mother and sister. This brought her great emotional pain and distress.
Back to work
After some time, Ms Jonas resumed work at the school where she was teaching, even when she was still on diapers and a catheter.
She alerted the school administration about her condition and she was allowed to go home frequently, during the office hours, for the purposes of changing her diapers.
The specialist
Ms Jonas was referred to see a specialist, who saw her on March 1, 2013. The specialist confirmed that she, indeed, had developed a fistula and thereafter continued to attend to her.
The specialist eventually removed the catheter as the leakage had subsided, but directed her to continue using diapers. The specialist informed her that their hospital did not have all the necessary equipment to rectify her injury but referred her to South Africa for specialised treatment.
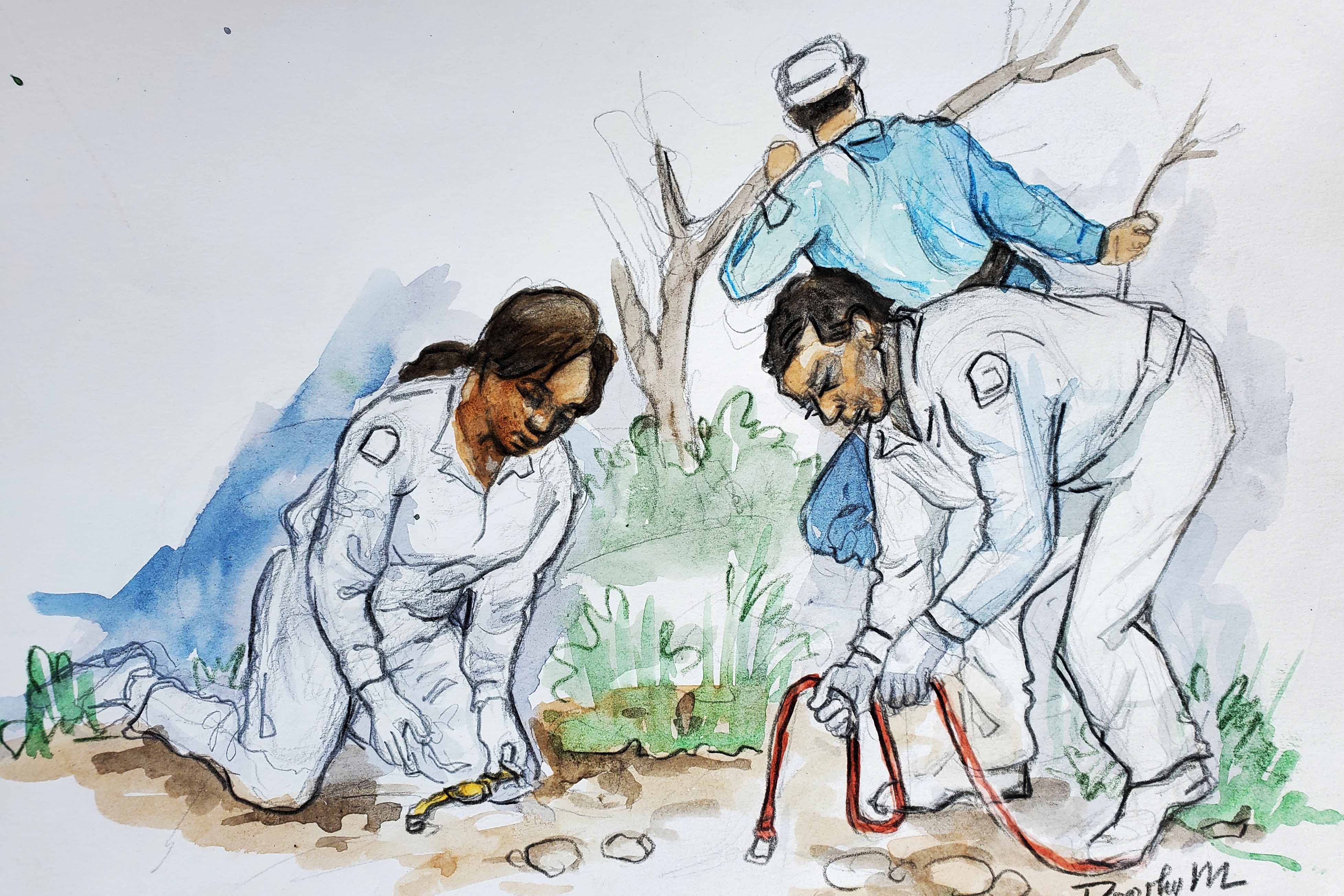
On March 18, 2013, the patient went to Pretoria Urology Hospital where she was attended to. In the hospital, it was found that the leakage of urine she had experienced and was still experiencing was the result of two injuries; one was an injury to the urether and another, an injury to the bladder.
The injury to the urether had healed but the one of the bladder was still healing. The injury to the bladder was repaired.
Ms Jonas filed a civil suit of medical negligence against the Attorney General as she had been operated on in a government hospital. She sought payment of the equivalent of Shs600m and the costs of the suit.
The injury to the bladder was repaired.
To be continued
Dr Sylvester Onzivua
Medicine, Law & You