Prime
Sex linked to some cancers
Cancer cell (white) being attacked by two cytotoxic T cells (red) that kill target cells bearing specific antigen while sparing neighboring uninfected cells. Photo/Courtesy
What you need to know:
- Data from the World Health Organisation (WHO) show that among the top ten cancers in the country, at least four are linked to sexually transmitted infections (STIs) such as Human Papillomavirus (HPV), HIV and Hepatitis B virus
Sexually transmitted infections remain one of the leading risk factors for cancer in Uganda, signalling a need to step up the fight against these diseases amidst campaigns focusing on healthy lifestyles, health specialists have said.
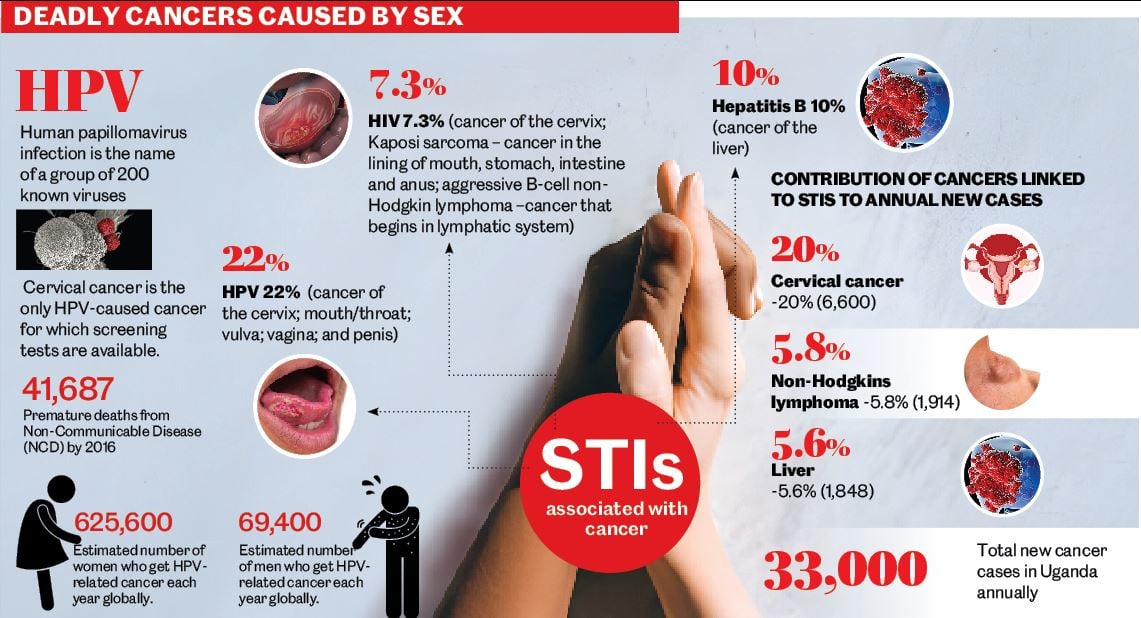
Data from the World Health Organisation (WHO) show that among the top ten cancers in the country, at least four are linked to sexually transmitted infections (STIs) such as Human Papillomavirus (HPV), HIV and Hepatitis B virus.
The WHO, in their 2020 report, indicated that cervical cancer, which is caused by infection with HPV, was the most common cancer, accounting for 6,959 (20 percent) of the 34,000 new cancer cases.
Kaposi sarcoma; a cancer in the lining of the mouth, stomach, intestine and anus, which is HIV-associated, came second, contributing 13 percent of the cancers.
These were followed by liver cancer, which is linked to the Hepatitis B virus, and Non-Hodgkin lymphoma that begins in the human lymphatic system and is associated with HIV.
As Uganda joins in global commemoration of World Cancer Month this February, it is sobering that the WHO report identified 35 different types of cancers in Uganda. Among them, cervical cancer, which is caused by the sexually transmissible HPV, was the leading cause of cancer-related death, killing 4,607 patients. The disease also has associations with HIV infection.
HPV-associated cancer
“The HPV is sexually transmitted,” Dr Martin Origa, a specialist in cancer of the female reproductive system affirms. “Most of the people who develop this type of cancer (cervical cancer) are those sexually active –it is never seen in those sexually naïve.”
Information from the WHO explains that HPV is the name given to a group of 200 known virus strains. Not all of these viruses are harmful to people. It is the high risk strain, which is deadly. The global health agency also states that in 90 percent of people the body controls HPV infection by itself.
“Persistent HPV infection with high-risk HPV types is the cause of cervical cancer and is associated with cancers of the vulva, vagina, mouth/throat, penis and anus. HPV usually goes away on its own without treatment. Others can cause abnormal cells to develop, which go on to become cancer,” reads the information from the WHO.
The WHO has reported elsewhere that women with HIV/Aids are six times more likely to develop cancer of the cervix than those who are HIV-negative.
“The presence of HIV infection weakens the immune system, making individuals more vulnerable to infection with HPV, and also to progression of HPV-related disease [such as cancer],” the WHO explains.
Uganda’s Health ministry has indicated that the prevalence of HPV and HIV in Uganda stands at 22 percent and 7.3 percent, respectively. The Uganda Aids Commission reported last year that annual new HIV infections are around 50,000.
However, according to information from the WHO and the National Cancer Institute (NCI) of America, in addition to cervical cancer, HIV infection is also associated with Kaposi sarcoma and aggressive B-cell Non-Hodgkin lymphoma.
Dr Alfred Jatho, the Uganda Cancer Institute (UCI) head of community cancer services, told Daily Monitor yesterday that the government is doing a lot of work to combat cervical cancer and other cancers linked to sexually transmitted diseases.
“Apart from targeting the population with the vaccine, we also educate people about how they can avoid the virus through safe sexual practices like the use of condoms,” he said.
However, WHO has cautioned that “condoms help prevent HPV but do not offer total protection because they do not cover all the genital skin.”
The agency also underlines that there is no cure for HPV infection.
Dr Jatho said the current directive from the government is that vaccination targets girls aged 10 years because it is meant for those who are sexually naïve. He said people can get HPV vaccines from public health facilities or during school outreaches.
Uganda, according to UNIPH, introduced the vaccine in 2014.
Dr Michael Baganizi, the head of the immunisation programme at the ministry, confirmed earlier last year the uptake of the two-dose HPV vaccine is not at the required level. The second dose is given after six months.
“Vaccination of persons above one and two years age bracket is a kind of new phenomenon for most people. So we need to educate people to embrace such vaccination. ,” he said.
Dr Jatho on the other hand asked women aged 25 years and above to do cervical cancer screening at least once every three years for early detection of the cancer. He said when the cancer has spread, the possibility to treat and cure a patient becomes hard and saving their lives is very difficult.
Hepatitis B and C-linked cancer
Hepatitis B and C are transmitted through contact with blood and body fluids from someone infected.
“This happens through sexual intercourse or blood transfusion. Blood in Uganda is screened for hepatitis B and C before it is used for transfusion. We also have mother-to-child transmission where the ministry is giving medicine for preventing mother-to-child transmission,” says Dr George Patrick Akabwai, a physician working at Baylor Uganda.
Dr Akabwai further explained that while treatment for hepatitis B is available, he said, it is not as a cure but to prevent the progression of the disease to conditions such as liver scarring, and eventually liver cancer.
HIV-associated cancers
According to information from NCI, people infected with HIV have a substantially higher risk of some types of cancer compared to uninfected people of the same age.
These, the institute said, include: “Kaposi sarcoma, aggressive B-cell Non-Hodgkin lymphoma, and cervical cancer. A diagnosis of any of these cancers in someone infected with HIV confirms a diagnosis of Aids.”
“Compared with the general population, people infected with HIV are currently about 500 times more likely to be diagnosed with Kaposi sarcoma, 12 times more likely to be diagnosed with Non-Hodgkin lymphoma, and, among women, three times more likely to be diagnosed with cervical cancer,” the NCI said.
The viruses that are most likely to cause cancer in people with HIV are Kaposi sarcoma-associated herpes virus, Epstein-Barr virus, which causes some subtypes of Non-Hodgkin and Hodgkin lymphoma, according to the institute.
“HIV-infected persons are more likely to be infected with these viruses than people in the general population,” NCI added.
Cancer patients speak
In July Last year, Ms Yesenta Kyasiima, 45, a resident of Bukiro in Mbarara district was diagnosed with cervical cancer at Mbarara Regional Referral Hospital.
She said that this was after she felt pain and discomfort in her private parts and went for infection treatment. However, the pain did go away despite treatment and she soon started releasing a smelly bloody discharge that she could not contain.
She was advised to go for cervical cancer screening at the referral hospital where she was diagnosed with cancer and was given some treatment.
Ms Kyarisiima said doctors referred her to Uganda Cancer Institute.




