Prime
UCI overwhelmed as cancer cases increase

Patients at the verandah of Uganda Cancer Institute in Mulago on Tuesday. PHOTO | SYLIVIA KATUSHABE
What you need to know:
- Although the general ward has always been congested, Dr Bukenya says the private ward only started seeing significant increases in the number of patients around January.
Manuela Akello, from Lira City, says her father has been at the Kampala-based Uganda Cancer Institute for over three months now. “My father has cancer in the stomach. He was operated three times; he had difficulties in passing out stool and had a problem in the intestines,” Akello narrates.
She says her father, Michael Ogwal Achonga, was at St Francis Hospital Nsambya for two months before he was referred to Uganda Cancer Institute (UCI) in May. “UCI doctors managed to rectify it [the problem]. We got the best treatment here and he is now able to ease himself. The treatment is ongoing and there is an improvement,” Akello adds.
Dr Jonathan Bukenya, the cancer specialist-in-charge of the UCI private ward, says the ward is full.
“We have bounced back eight patients today (Tuesday). We can accommodate 25 patients and all our rooms are full. The private ward should be expanded to meet the demand,” Dr Bukenya says.
The general bed capacity for both private and general patients is 100, according to information from the management. Up to 200 patients are handled daily at the facility –both outpatients and inpatients.
Although the general ward has always been congested, Dr Bukenya says the private ward only started seeing significant increases in the number of patients around January.
“They are coming because of the new services, and improvement in quality of care and customer experience. People are no longer going abroad for cancer care,” he explains.
Dr David Miti, a cancer specialist at UCI, says they have introduced modern machines to improve efficiency in cancer care and reduce side effects of treatment.
“The new machine is called Linear Accelerator Machine (LINAC). We have had one working but they have introduced more. The way it works is that when you have a tumour, we place you on that machine and then the radiation from the machine is directed to the tumour to ‘dissolve’ that tumour,” he explains.
“The other machine called the cobalt machine could burn tissues around the tumour [thus increasing side effects of treatment] but the LINAC maps exactly the area with the tumour and treats it without affecting tissues around. Not all services are private, those who can’t afford private ward, use general ward,” he adds.
According to cancer specialists, the LINAC machine helps patients heal in fewer radiotherapy sessions like one to five, compared to other machines where one undergoes 20 to 40 sessions. The number of sessions depends on the type and extent of the tumour. The specialists also say shorter sessions lower the risk of side effects and reduce time spent on treatment.
Dr Miti also notes that there is a general spike in the number of people developing cancer.
“The other thing is that people have become more aware of cancer because of the sensitisation by UCI and partners. There are so many cases picked up in the screening we do across the country,” he says.
“All of them were being referred here but UCI has opened up a branch in Gulu and most of the cases from northern Uganda will be handled there. Previously, we could see 5,000 new cases in a year but as I talk, by June, we crossed the 4,000 mark of new cases, this is close to the number we would see in one year,” he adds.
Government statistics indicate that in 2010, there were 2,037 new cancer cases, which means the numbers in six months of 2023, are double the numbers seen in the entire 2010 or more than four times the numbers seen in half of 2010.
According to statistics from the International Agency for Research on Cancer, there were 34,000 new cancer cases in Uganda in 2020 and of these, 22,000 died. However, majority die in communities as they don’t seek cancer treatment in designated facilities.
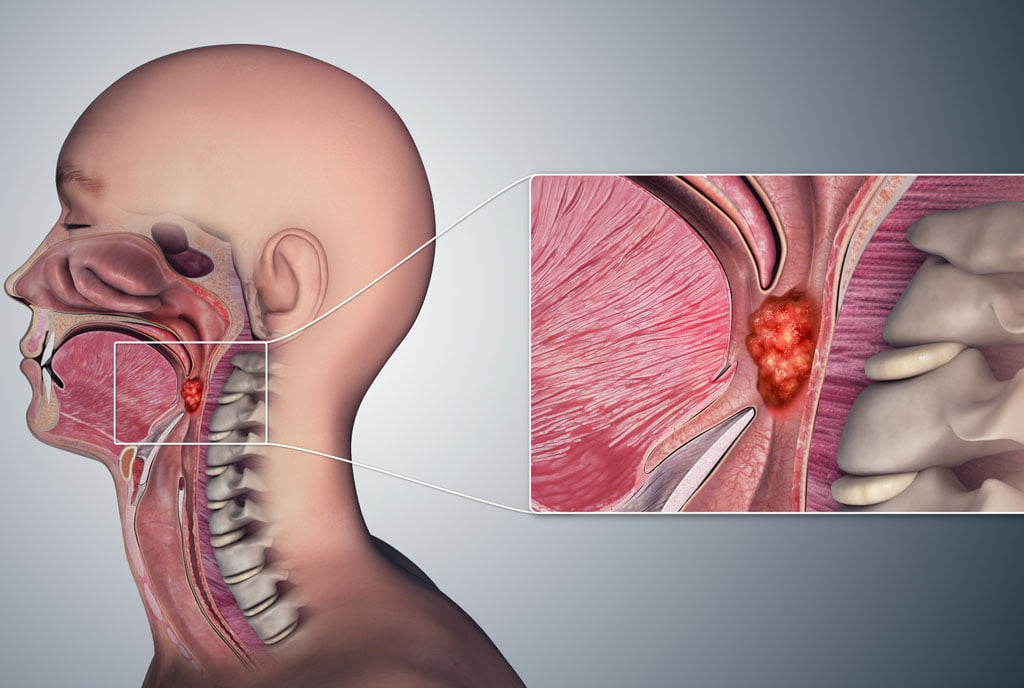
Dr Miti says they are seeing, “a rise in gastro-intestinal malignancies –which is cancer of the esophagus (throat), stomach and colon (intestine), and liver. But generally, prostate cancer and then breast cancer and cervical cancer are common in females.”
He adds: “The only thing limiting us is the space. There is a new building here that is being constructed at a very high speed and there are more people specialising in cancer. With this, we believe there will be more space and human resources to handle cancer patients.”
Ms Christine Namulindwa, the spokesperson for UCI, says the new building will have 360 beds for both general and private patients. Namulindwa also says the UCI and partners have been running campaigns to promote the prevention of cancer and encourage people to seek early diagnosis and treatment.
Dr Bukenya says the private patients meet some charges. “We have shared rooms (with three patients) and single rooms. For shared rooms, they pay Shs100,000 per day. The payment for a self-contained single room is Shs180,000. The charges are for amenities and care from doctors and nurses. But treatment is free,” he adds.
However, Kellen Komujuni, from Mbarara, a caretaker, who is also at the private ward, says they always buy some medicines.
“We were transferred here after spending two days in Mbarara. My patient has breast cancer,” Ms Komujuni narrates.
“We have been here for one week and the services are good. Whenever there is an emergency, the doctors come in promptly and help. In their (UCI) pharmacy, you get some medicines free but you buy others from First Pharmacy. Medicine for cancer is expensive but we are managing,” she adds.
A joint report by Makerere University and UCI researchers, released in February, indicates that to access treatment and care at UCI, cancer patients spend an average of Shs300,000 on a single visit, although some spend as high as Shs800,000.
The study titled: “Impoverishing and Catastrophic Health Expenditure on Cancer Care among Persons Affected by Cancer in Uganda”, was conducted in 2021 during the Covid-19 pandemic lockdown.
According to researchers, the money is used to purchase drugs for the UCI, imaging services, and tests, among others. The imaging and tests are done within or outside UCI depending on the availability of services and equipment.
“Overall, at least half of all cancer patients experienced catastrophic health expenditure on cancer care and treatment. Five of 10 patients spent at least 40 percent of their household income on cancer health care,” the report reads in part.
However, Dr Jackson Orem, the executive director of the UCI, says the institute has seen improvement in the availability of essential medicines.
“The UCI has put measures in place to ensure medicines are readily available to all patients, both young and old, at no cost. We are working directly with manufacturers and eliminating middlemen, something that has enabled us to achieve free access to medicines without drug stockouts,” he says.
In May, an international study ranked UCI as the best public facility in East Africa regarding uninterrupted access to essential cancer drugs. The study was conducted in eight cancer treatment centres in Kenya, Tanzania, Rwanda and Uganda between 2020 and 2022.
The rankings were as follows Aga Khan University Hospital (15 percent), UCI (19 percent), Kenya’s Moi University Teaching and Referral Hospital (21.6 percent) and Tanzania’s Muhimbili National Hospital (23.7 percent).
This was followed by Tanzania’s Bugando Medical Centre (32.3 percent), Rwanda’s Butaro Cancer Centre of Excellence (39 percent), Kenyata National Hospital (44.5 percent) and Jaramogi Oginga Odinga Hospital (48.5 percent). In Uganda, five cancer drugs out of 27 medicines were not available.
Dr Jane Ruth Aceng, the Health Minister, says the government made UCI an autonomous body and that increased efficiency in procuring medicines and care for patients.
She says the availability of cancer drugs at the institute is at 90 percent. “There is a potential to hit 100 percent [in terms of availability of essential cancer drugs],” she says.
Dr Charles Ayume, the head of the Parliament Committee on Health, says the establishment of regional cancer centres is also being expedited to minimise congestion at UCI.
“It’s true that the UCI is overloaded with too many patients and this has outrun the space and the human resource. The government’s strategic direction is to decentralise cancer services to regional cancer centres in Mbale, Mbarara, Gulu and West Nile,” he says.
The general ward and outpatient units have a large number of patients, with some sleeping on the floor or standing as they wait for space.
“Some of the veranda cases at UCI are patients who have accessed care and are waiting for their next round of chemo or radiotherapy,” Dr Ayume says.
“They can’t afford the high return journey transport costs to up-country destinations. Regional cancer centres will address some of these issues. The government will continue to support doctors willing to specialise in oncology,” Dr Ayume notes.
Government statistics show that “UCI is understaffed with a doctor-patient ratio at 1:100, nurse-patient ratio at 1:50.”
Dr Orem reveals that the government has already cleared the northern regional cancer centre to handle patients ahead of commissioning in November. The centres like Mbarara also offer some basic cancer services such as screening.
“The functionalisation [of the centre] has started. Patients can go there now. Any care can be accessed there except radiotherapy. All the basic things can be done there,” Dr Orem says.
“We will do cancer screening, diagnosis, investigations, treatment, follow-up, admissions, emergencies and also the element of referrals,” he adds.
The Shs30 billion Northern Regional Cancer Centre, in Omoro District, has 100 beds with state-of-the-art equipment for the diagnosis and skilled staff, according to the UCI.
Drivers of cancer
Dr David Miti, a cancer specialist at UCI, says one of the major drivers of cancer is lifestyle.
“We are becoming more sedentary where people don’t do [physical] exercises. People eat so much processed foods, a problem which is worsened by rapid urbanisation,” he says.
The expert says there are diseases that also increase one’s risk of developing cancer. “The Kaposi sarcoma which affects the skin and the lining of the mouth, digestive system and the lungs, comes as a result of HIV. However, some other forms of the same cancer are not caused by HIV. And you see that HIV is still prevalent in the country,” Dr Miti says.
“The human papillomavirus is responsible for cervical cancer and HIV is a contributing factor. People get ulcers, they don’t treat them (they don’t heal) and the ulcers turn into cancers. People have hepatitis, they don’t treat and this can progress into liver cancer,” he adds.
Dr Miti advises people to go for regular checkups for early detection so it can be treated successfully.
“For men who are 40 years and above, you must have a checkup for prostate cancer because you are more susceptible to that form of cancer. You should also be very cautious and don’t downplay what you don’t understand,” he says.
“You should go to the hospital to find out what is happening to you. The chance of healing from cancer is very high when it is an early stage –like stage one. Most people who are dying are coming at late stage and you don’t have much you can do to save them,” he adds.