Prime
Here’s how to reduce maternal deaths

Judith G. Amoit
What you need to know:
...translating this potential into tangible outcomes requires concerted efforts from policymakers, healthcare professionals, and community stakeholders alike.
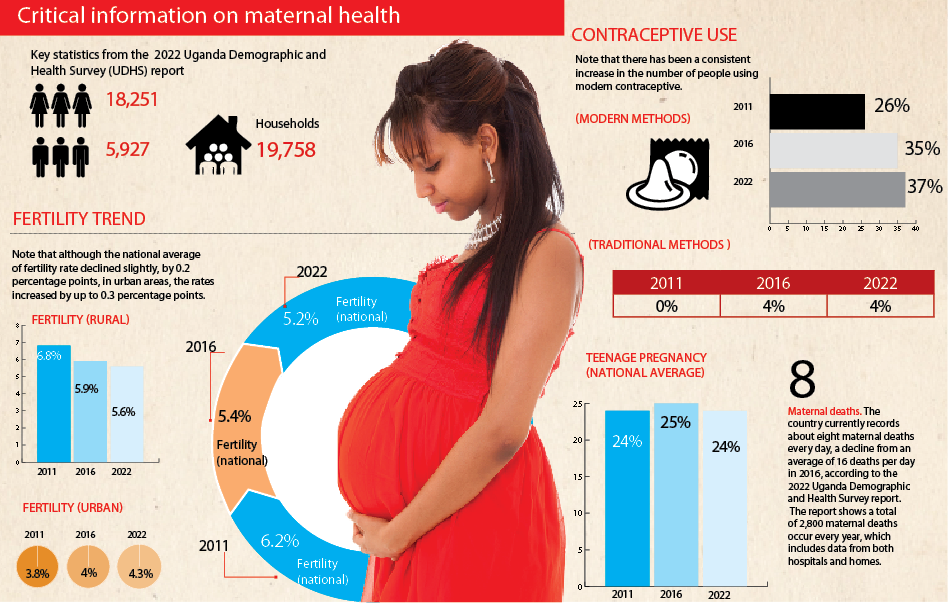
According to the recent Uganda Demographic Health Survey 2022 results (UDHS) maternal mortality ratio declined from 336/100,000 live births in 2016 to 189/100,000 live births as of 2022.
Despite commendable efforts to improve maternal health outcomes, challenges persist, hindering the nation’s progress towards achieving Universal Health Coverage (UHC) and the Sustainable Development Goal. However, amidst these challenges lies a vital trio; blood, functional referral system and skilled healthcare. These elements, when harnessed effectively, have the potential to improve maternal healthcare and propel Uganda towards the realisation of UHC and SDGs.
Firstly, blood plays an important role in addressing maternal health complications, particularly obstetric hemorrhage, a leading cause of maternal mortality in Uganda.
However, blood shortages and inadequate infrastructure for blood banking persist as formidable barriers.
To address this, strategic investments in blood collection, testing, and distribution infrastructure are imperative. Furthermore, robust community-based blood donation programmes coupled with effective coordination between health facilities and blood banks can ensure a steady supply of safe blood, thereby mitigating maternal mortality due to hemorrhage.
Secondly, functional referrals are indispensable in ensuring that pregnant women receive timely and appropriate care, especially in cases requiring specialised interventions beyond the capacity of primary healthcare facilities. Life-threatening obstetric complications usually lead to the need for referral and constitute the commonest direct causes of maternal deaths. Urgent management of referrals can potentially lower the maternal mortality rate.
Unfortunately, delays in referrals significantly contribute to adverse maternal outcomes. Strengthening referral systems through improved communication channels, enhanced transportation networks, and capacity-building initiatives for healthcare providers is essential. Moreover, leveraging technology, such as telemedicine and mobile health applications, can facilitate swift and accurate referrals, bridging geographical barriers and ensuring equitable access to maternal healthcare services across Uganda.
Thirdly, skills acquisition among healthcare providers is paramount in enhancing the quality of maternal healthcare delivery.
However, the shortage of skilled healthcare professionals, particularly midwives and obstetricians, remains a pressing issue. To address this, comprehensive training programmes, continuous professional development initiatives, and incentive schemes are indispensable. Additionally, fostering interdisciplinary collaboration and mentorship programmes can harness the collective expertise of healthcare teams, thereby optimising maternal health outcomes.
The convergence of evidence-based interventions centred on blood, referrals, and skills holds immense promise for advancing maternal healthcare in Uganda and achieving Universal Health Coverage together with Sustainable Development Goals. However, translating this potential into tangible outcomes requires concerted efforts from policymakers, healthcare professionals, and community stakeholders alike.
Ms Judith Grace Amoit is the communications officer, Digital Payments Project.