Prime
Why you must know your rights as a patient

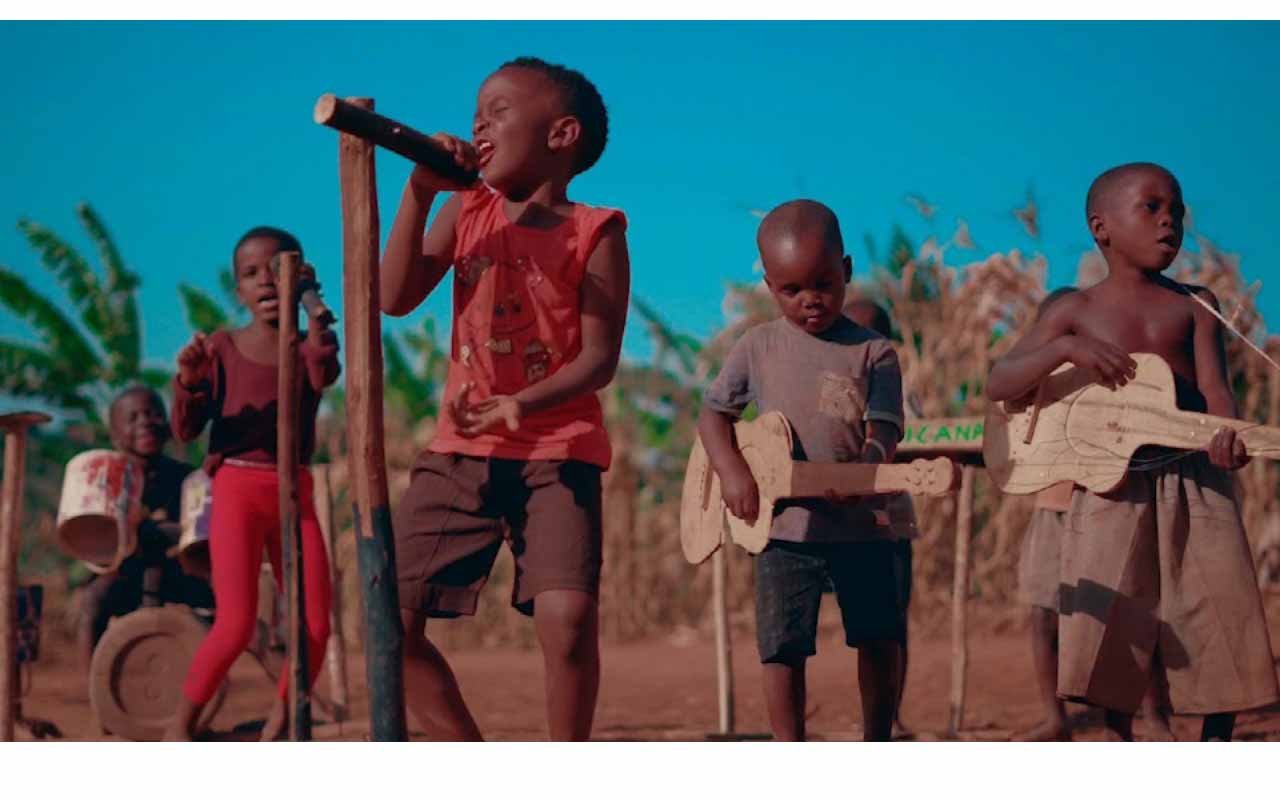
Everyone should have a fair and just opportunity to achieve good health and well-being. PHOTO | COURTESY | healthline.com
What you need to know:
- On April 7 every year, the World Health Day (WHD) is commemorated to highlight priority areas of public health concern in the world and address them. According to the World Health Organisation (WHO), this year, the day was celebrated under the theme 'My health, my right’.
Around the world, the right to health for millions of people is increasingly coming under threat. Diseases and disasters loom large as causes of death and disability. Conflicts are devastating lives, causing death, pain, hunger and psychological distress.
The burning of fossil fuels is simultaneously driving the climate crisis and taking away our right to breathe clean air, with indoor and outdoor air pollution claiming a life every five seconds.
The World Health Organisation (WHO) Council on the Economics of Health for All, has found that at least 140 countries recognise health as a human right in their constitution.
Yet, countries are not passing and putting into practice laws to ensure their populations can access the needed health services. This indicates that at least 4.5 billion people, which is more than half of the world’s population, were not fully covered by essential health services in 2021.
According to the WHO website, “This year’s theme was chosen to champion the right of everyone, everywhere to have access to quality health services, education, and information, as well as safe drinking water, clean air, good nutrition, quality housing, decent working and environmental conditions, and freedom from discrimination.”
But what is quality of care?
According to the WHO, quality of care is the degree to which health services for individuals and populations increase the likelihood of desired health outcomes. It is based on evidence-based professional knowledge and is critical for achieving universal health coverage. As countries commit to achieving health for all, it is imperative to carefully consider the quality of care and health services.
The Ministry of Health (MoH) defines quality of care as “the extent to which health care services provided to individuals and patient populations improve desired health outcomes. In order to achieve this, health care must be safe, effective, timely, efficient, equitable and people-centred.”
Access to health care
In Uganda, many health facilities and hospitals are located in urban centres, which increases access to health care although the out-of-pocket expenditures are still high.
According to the International Journal for Equity in Health, rural access to health care remains a challenge in Sub-Saharan Africa due to urban bias, social determinants of health and transportation-related barriers.
“Health systems in Sub-Saharan Africa often lack equity, leaving disproportionately less health centre access for the poorest residents with the highest health care needs. Lack of health care equity in Sub-Saharan Africa has become of increasing concern as countries enter a period of simultaneous high infectious and non-communicable disease burdens, the second of which requires a robust primary care network due to a long continuum of care,” reads part of the journal.
Efforts
According to Dr Martin Ssendyona, the head of department for the standards compliance and patient protection at the MoH, the government of Uganda is doing all it can to increase access to health service among the people.
“We have a decentralised system of health care and all the 16 regions of the country have a regional referral hospital that manages big health concerns. Then, there are health centre IVs, IIIs and IIs where people can access free health care. These also work in collaboration with the village health teams of trained health care providers who live within the communities,” he says.
In a bid to increase access to health care for all and reduce out of pocket expenditures on health care, the MoH proposed the National Health Insurance Scheme (NHIS).
The draft stipulates that all Ugandans above the age of 18 should enroll and pay a premium to the proposed NHIS, according to their ability. This will enable them access packages from accredited public and private health facilities using a card.
Discussions about the National Insurance scheme in Uganda started in the 1980s and slowly evolved over years. Last year, consultations about the scheme were finalised and the bill was drafted. It is now before the cabinet awaiting approval, according to the spokesperson at MoH.
Private health centres
When it comes to private health care centres, Dr Ssendyona remarks that these centres must be registered and given a practicing license.
“Depending on the services they are designated to offer, they should belong to the nurses and midwifery council, Allied Health Professionals Council, pharmaceutical society of Uganda, Uganda Medical and Dental Practitioners Council and many others,” he says.
These associations help assess the implementation of services in private health care centres. They do the monitoring and evaluation of services offered and measure the quality of services.
The right to feedback
The WHO recommends developing and implementing national quality health service standards and monitoring systems as one of the actions necessary to make progress toward universal health coverage by 2030. The MoH in Uganda developed a comprehensive service standard manual that must be followed by all the health care facilities.
Ssendyona says the manual defines the type of services that must be offered at the different levels of health care. If a patient is not satisfied by the services a health care centre offers, they should speak up and give feedback to the immediate person in charge of the facility. Here they will get immediate help and feedback.
The Comprehensive Health Service standards Manual is also aimed at ensuring that patients and service users receive comprehensive health care that meets their individual needs and considers the impact of their health issues on their life and wellbeing. Also, there is the patients’ rights and responsibility charter that spells out the various patient rights and responsibilities for the service consumers in the national health care system.
“The charter empowers communities to demand for quality care from service providers for both private and public health care centres. It also ensures that patients comply with the instructions and guidance given to them by the health service providers,” Dr Ssendyona says.
Client charter
The client charter was introduced under the public service reform programme as a tool to strengthen the demand for accountability for service delivery in the health system, says the minister of health Jane Ruth Aceng.
“This charter spells out the roles and responsibilities and commitments of the MoH to their clients in the public and private sector, at the national, regional, district, health facility, community and individual levels,” Dr Aceng says.
The challenges
The National Institute of Health points out that the factors that affect the quality of services delivered by health facilities in Uganda include inadequate numbers of trained health workers, shortage of essential drugs, poor attitude of the health workers, high health costs, and long distances to health facilities, especially in the rural areas.
Dr Ssendyona emphasises the need for the government to provide funds to maintain facilities, address human resource shortages, provide medical supplies and keep the facilities well equipped.