Prime
Govt to combine HIV treatment with non-communicable diseases
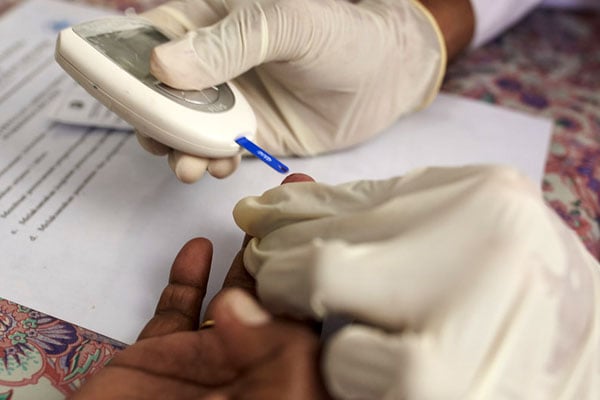
The Health Ministry has said it is running pilot projects in some health facilities to determine ways of including treatment for non-communicable diseases to usual HIV/Aids treatment so as to curb deaths among the patients.
The Health Ministry has said it is running pilot projects in some health facilities to determine ways of including treatment for non-communicable diseases to usual HIV/Aids treatment so as to curb deaths among the patients.
Uganda lost 21,000 HIV patients in 2019, according to statistics from the Uganda Aids Commission (UAC).
According to the Makerere University Joint Aids Programme (MJAP), a large number of the deaths was due to untreated non-communicable diseases among the patients.
Dr Joshua Musinguzi, the Aidscontrol programme manager at Ministry of Health, last week told Daily Monitor that the integration of the services is one of the most important plans they intend to roll out countrywide.
“We want to ensure that health care workers are able to provide both services. If a patient has come to pick their drugs [ARVs], you don’t want to tell them to come back the next day for NCDs treatment,” Dr Musinguzi said.
“We have been designing mechanisms to ensure that we train our health workers to provide holistic care. The antiretroviral treatment (ART) has enabled people to live long, but as you grow old, the NCDS start coming, we are encouraging the integration in our guidelines,” he said.
Dr Musinguzi said some studies have demonstrated a link between drugs used to treat HIV with conditions like obesity.
He added that the pilot study to determine how best to integrate the services is being done by the ministry alongside Uganda Virus Research Institute, The Aids Support Organisation and other institutions under the support of the European Union.
Earlier, Dr Martin Muddu, the care and treatment adviser at the HIV clinic for outpatients at Mulago National Referral Hospital, said a quarter of the 17,000 patients they see annually have high blood pressure, a condition that puts them at higher risk of death.
“The quality of care for HIV/Aids patients in most health facilities is good. They are getting virological suppression and most of them are not dying of Aids-related illnesses,” Dr Muddu said.
He added: “But most of the patients are dying of NCDS and majority of the deaths are due to high blood pressure. HBP if not treated, leads to complications like stroke, heart disease, kidney disease and others.”
Dr Muddu said integrating the treatment for hypertension treatment with HIV care has curbed deaths among the patients.
“We have 1,135 people living with HIV/Aidswho also have hypertension and they are receiving integrated care in this clinic where they are given the anti-retroviral (ARV) medicine and that for hypertension.”
“Those receiving integrated care have been to achieve up to 75 per cent of hypertension control, from the baseline figure of less than 5 per cent. We only lost four of them during lockdown because they couldn’t travel to come and pick their medicines for hypertension but they were getting ARVs from nearby health facilities,” he said.
Dr Fred Semitala, the acting executive director of MJAP, said the scale-up of the integration will require the government to equip all health facilities with essential equipment for diagnosing NCDS .



