Prime
Uganda questions WHO’s excess Covid deaths tally

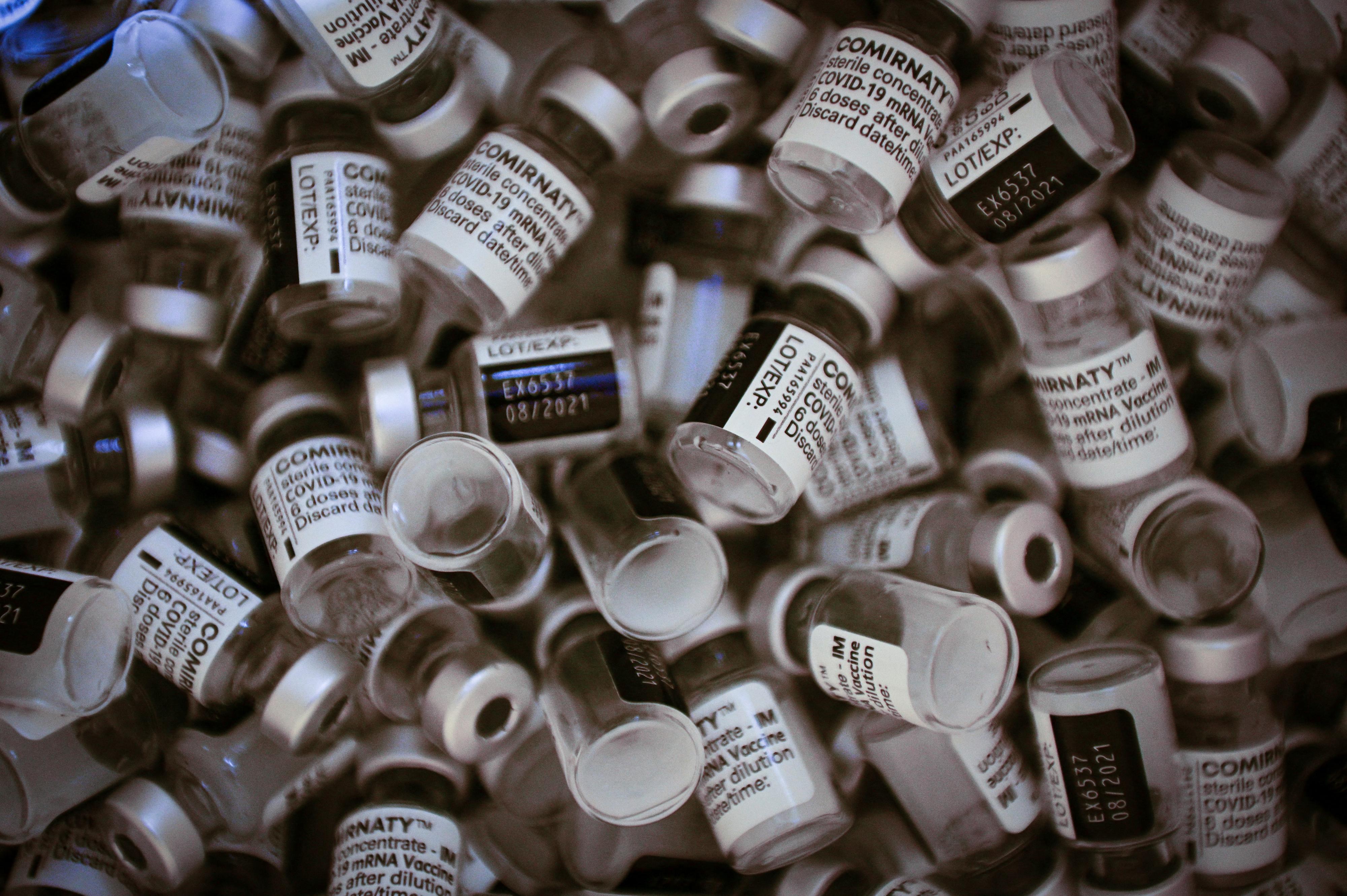
A man receives a Covid-19 jab in Kampala last year. Uganda has been applauded for keeping Covid-19 deaths low through the tough control measures such as vaccination, among others. PHOTO | FILE
What you need to know:
- The global health agency, specifically on the statistics for Covid-19 deaths, said the data which was based on mathematical modelling is very reliable. But the Director of Public Health, Dr Daniel Kyabayinze, challenged the WHO modelling and the estimates.
New statistics from the World Health Organisation (WHO) indicate that there were 20,519 excess deaths in Uganda associated with the Covid-19 pandemic before 2022.
However, officials at the Ministry of Health have questioned the methodology the world health body used to reach the excess deaths figure.
The ministry’s official figures indicate that Uganda had registered 3,302 deaths from 144,540 infections by the end of 2021.
The WHO says excess mortality statistics include deaths associated with “Covid-19 directly (due to the disease) or indirectly (due to the pandemic’s impact on health systems and society).”
It also adds that Uganda’s Covid-19 deaths were under reported. By the end of 2021, the WHO says up to 65 percent of Africans, including about 27.3 million Ugandans, had been infected by Covid-19 since the outbreak.
The agency said testing was extremely low across the globe and so most cases went undetected. This figure means Uganda didn’t report 95 percent of Covid-19 infections.
The global health agency, specifically on the statistics for Covid-19 deaths, said the data which was based on mathematical modelling is very reliable. But the Director of Public Health, Dr Daniel Kyabayinze, challenged the WHO modelling and the estimates.
“They should show us where the graves [of the excess deaths] are. The official statistics of confirmed Covid-19 deaths in the country are there. We worked hard to keep Covid-19 mortality low. The people who are extrapolating the data are the same people who refused to give us vaccines,” he told Sunday Monitor.
Uganda has been applauded for keeping Covid-19 deaths low through the tough control measures, including the then highly disputed closure of schools, and dusk-to-dawn curfews.
WHO explains new figures
Dr Tedros Adhanom Ghebreyesus, the WHO director-general, said in a statement last week: “These sobering data not only point to the impact of the pandemic but also to the need for all countries to invest in more resilient health systems that can sustain essential health services during crises, including stronger health information systems.”
In the same statement, the WHO said most of the excess deaths (84 percent) are concentrated in South-East Asia, Europe, and the Americas.
The statement said excess mortality (unreported deaths) is calculated as the difference between the number of deaths that have occurred and the number that would be expected in the absence of the pandemic based on data from earlier years.
The WHO revealed that the production of these estimates is a result of a global collaboration supported by the work of the Technical Advisory Group for Covid-19 Mortality Assessment, and country consultations.
The agency said this group—convened jointly by the WHO and the United Nations Department of Economic and Social Affairs (UNDESA)—consists of many of the world’s leading experts, who developed an innovative methodology to generate comparable mortality estimates even where data are incomplete or unavailable.
“This methodology has been invaluable as many countries still lack capacity for reliable mortality surveillance and, therefore, do not collect and generate the data needed to calculate excess mortality. Using the publicly available methodology, countries can use their own data to generate or update their own estimates,” the agency said.
Mr Stefan Schweinfest, the UNDESA director, said in last week’s statement: “Data deficiencies make it difficult to assess the true scope of a crisis, with serious consequences for people’s lives. The pandemic has been a stark reminder of the need for better coordination of data systems within countries and for increased international support for building better systems, including for the registration of deaths and other vital events.”
MoH officials weigh in
Dr Charles Olaro, the director of clinical services at the Health ministry, said they will examine the report. He added that it is possible that some Covid-19 deaths were not captured.
Dr Olaro, however, said the country did its best to curb Covid-19 spread and deaths through good patient management.
Mr Emmanuel Ainebyoona, the ministry spokesperson, said: “We had challenges with PCR testing. So, it is possible that some Covid-19 cases were not detected.”
Dr Henry Kyobe—the National Incident Commander for Covid-19—said the research they did earlier put the seroprevalence in the country at 22 percent. This means only 22 percent of Ugandans were exposed (infected) to Covid-19. The 22 percent is substantially less than the WHO estimate of 65 percent.
Seroprevalence is the percentage of people in a population who have antibodies against a specific infectious agent in their blood and this shows that they have been exposed to the agent.
So has Uganda reached herd immunity?
“The last sero survey we did in March 2021 before the emergence of Delta variant [which triggered the most deadly second wave of the pandemic in the country] found the prevalence at 22 percent. But the two waves, the second and third were much more aggressive, which pushed the seroprevalence much higher. We anticipate it to be very high, but I can’t attach a number to it,” Dr Kyobe told Sunday Monitor.
He added that although many people are exposed to Covid-19 and have developed some form of immunity, following the infection or through vaccination, the country has not yet reached herd immunity.
Herd immunity refers to resistance to the spread of an infectious disease within a population that is based on pre-existing immunity of a high proportion of individuals as a result of the previous infection or vaccination.
“It is possible that the previous exposure to the virus may be protective and may explain the drop in infections in the country,” Dr Kyobe explained, adding: “This protection becomes better when combined with vaccination. The current decline in infections could also mean the virus has already infected all the susceptible people. But we also have cases of reinfection and breakthrough infections.”